IBD is a chronic immune-mediated disease that requires continuous patient care. The frequent contact and the good relationship with the multidisciplinary team (MDT) are essential for improving quality of life (QoL) and medication adherence aiming at treatment success. The aim of the study was to assess the importance of MDT in the view of patients with IBD and its impact on QoL and in medication adherence.
MethodsA cross-sectional study was carried out, including 114 patients from an IBD reference center in Brazil. The relevance of MDT was assessed through a questionnaire that included the importance of physicians, nurses, nutritionists and psychologists in the patient care. QoL was assessed by IBDQ. Treatment adherence and knowledge about the disease were assessed using the Morisky and CCKNOW questionnaires, respectively.
Results: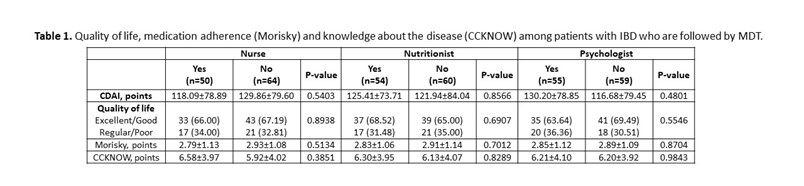 In total, 69 (60.53%) patients with CD and 45 (39.47%) patients with UC were included. The mean age was 39.16 (±13.50) years and 58.77% were female. The disease duration was 9.88 (±7.35) years. Presence of comorbidities was observed in 52.63% patients. About 57 (82.61%) patients with CD use biological therapy, with a statistical difference (p <0.0001) when compared to patients with UC (37.78%). The gastroenterologist was considered very important by 91.23% of patients, coloproctologist by 62.07% of patients, nurse by 65.05% of patients, nutritionist by 50% of patients and psychologist by 47.25% of patients. In the analysis of QoL, 24 (21.05%) patients had excellent QoL, 52 (45.61%) had good QoL, 29 (25.44%) had regular QoL and 9 (7.89%) had poor QoL, with no difference between patients who followed with nurses or other MDT professionals (Table 1). Medication adherence was low in 58.88% of patients. Knowledge about the disease was low (6.21 ± 3.99 points), being higher among patients with CD (p = 0.01). Patients identify the doctor as the main provider of care for their health, but about 10% leave with doubts from their appointments. 10% of patients think that more care with the nurse is necessary and less than 10% of patients are clarified by the nurse about QoL, ostomies, fecal incontinence, disease activity, biological therapy and sexuality.
In total, 69 (60.53%) patients with CD and 45 (39.47%) patients with UC were included. The mean age was 39.16 (±13.50) years and 58.77% were female. The disease duration was 9.88 (±7.35) years. Presence of comorbidities was observed in 52.63% patients. About 57 (82.61%) patients with CD use biological therapy, with a statistical difference (p <0.0001) when compared to patients with UC (37.78%). The gastroenterologist was considered very important by 91.23% of patients, coloproctologist by 62.07% of patients, nurse by 65.05% of patients, nutritionist by 50% of patients and psychologist by 47.25% of patients. In the analysis of QoL, 24 (21.05%) patients had excellent QoL, 52 (45.61%) had good QoL, 29 (25.44%) had regular QoL and 9 (7.89%) had poor QoL, with no difference between patients who followed with nurses or other MDT professionals (Table 1). Medication adherence was low in 58.88% of patients. Knowledge about the disease was low (6.21 ± 3.99 points), being higher among patients with CD (p = 0.01). Patients identify the doctor as the main provider of care for their health, but about 10% leave with doubts from their appointments. 10% of patients think that more care with the nurse is necessary and less than 10% of patients are clarified by the nurse about QoL, ostomies, fecal incontinence, disease activity, biological therapy and sexuality.
Patients considered doctors as the most important professionals in their care. Although the service has a multidisciplinary team, not all patients had the opportunity to consult with all professionals, mainly do the Covid pandemic in 2020 and 2021. The lack of contact with the entire team, especially with the nurse, may have contributed to low medication adherence and low knowledge of the disease, impacting disease control and QoL.
Data regarding the influence of prednisolone tapering on clinical outcomes among patients with ulcerative colitis (UC) are limited. We aimed to investigate the influence of different prednisolone tapering algorithms on the effectiveness of infliximab (IFX) among patients with UC.
MethodsThis Danish retrospective single-center study included all patients with UC who were treated with IFX between 2009 and 2019 at Herlev University Hospital. The patients were grouped according to the prednisolone tapering: standard (≤5 mg/week), fast (>5 mg/week), or direct discontinuation after an initial course of less than one week. Finally, we included a control group of patients treated with IFX monotherapy. The primary outcome was corticosteroid-free clinical remission at weeks 14 and 52 defined as a partial Mayo score ≤1. Variables with a p-value ≤0.20 in univariable regression analysis were included in multivariable analysis. A subgroup analysis containing patients with acute severe ulcerative colitis (ASUC) treated with at least 40 mg of prednisolone at initiation of IFX was performed.
The study included 148 patients with UC of whom 81 (54.7%) were treated with prednisolone at the initiation of IFX. No association between prednisolone tapering and corticosteroid-free clinical remission with IFX at weeks 14 or 52 was observed (Figure 1 and Table 2). However, a higher proportion of patients in the standard tapering group achieved a C-reactive protein (CRP) level less than 5 mg/L at week 14 as compared with the fast-tapering group (23/23 (100%) vs. 14/18 (77.8%); p=0.03) and directly discontinuation group (6/10 (60%); p=0.03). This difference was not explained by prednisolone usage. In addition, none of the patients within the standard tapering regime (0/24; 0%) had severe activity at week 14 whereas this was seen in 4/19 (21.1%) in the fast tapering regime (p=0.03). In the subgroup analysis of 33 patients with ASUC, the standard tapering algorithm was associated with higher clinical remission as compared with the fast tapering regime at week 14 (9/14 (64.3%) vs. 5/19 (27.8%); p=0.02) and clinical response or remission at week 52 (12/14 (85.7%) vs. 7/19 (36.8%); p=0.01, Figure 2).
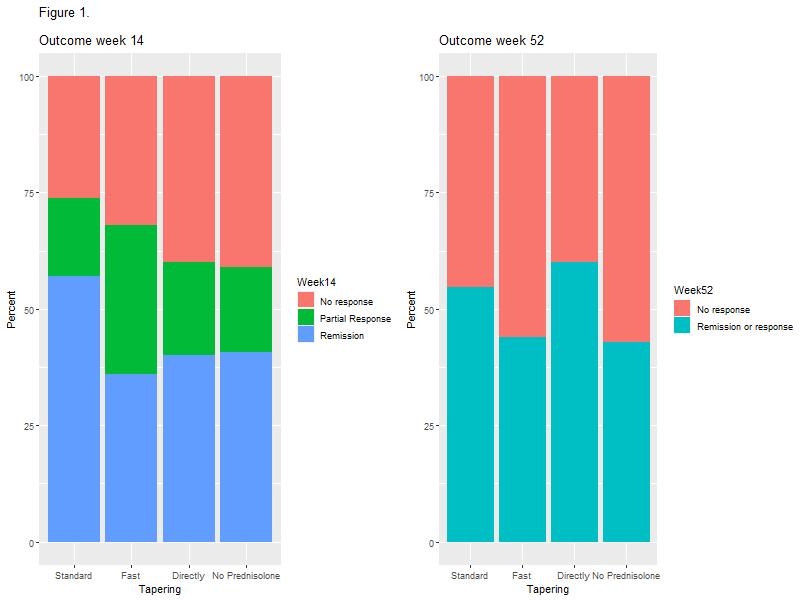
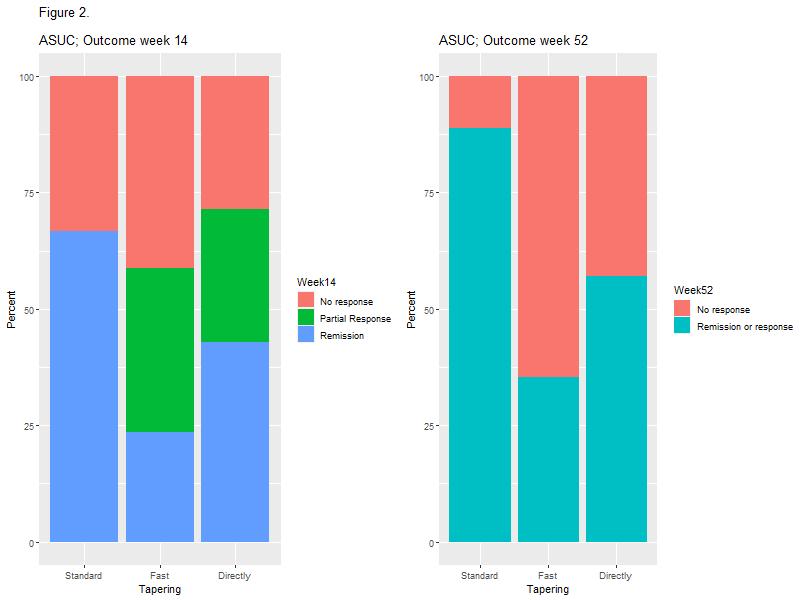
This study demonstrated no overall impact of prednisolone tapering algorithms on short and long-term effectiveness of IFX in patients with UC. However, standard tapering resulted in lower CRP levels and fewer cases of severe disease activity in the overall cohort and higher rate of short and long-term clinical response among ASUC patients, as compared with fast tapering regimes. Taken together, the data indicate that longer corticosteroid exposure in patients with high disease burden might improve IFX responses.
Educational objectives:
- To discuss the therapeutic options for paediatric patients with inflammatory bowel disease (IBD) refractory to standard medical therapy
- To review the current evidence for segmental resection for patients with Crohn’s disease (CD)
- To review the evidence for “out of the box” treatments such as tacrolimus for both diseases, thalidomide for CD, granulocyte- monocyte apheresis, fecal microbial transplantation, mesenchymal stromal or adipose cell therapy for refractory perianal fistulas, dual biologics and autologous hematopoietic stem cell transplant.
Presentation outline:
When patients with IBD fail standard medical therapies there are limited therapeutic options. The first step should be to optimize biologic therapy (based on therapeutic drug monitoring in anti-TNF treated patients or empiric escalation in patients treated with vedolizumab or ustekinumab). Tofacitinib should be considered for patients with ulcerative colitis (UC).
Surgical resection has an established benefit in segmental CD even in the colon.
The edition of nutritional therapy as a combination treatment with biologics may be considered for selected cases.
Tacrolimus was shown efficacious in UC and may serve as a bridge to other therapies such as vedolizumab or even in combination at low doses with vedolizumab.
Thalidomide was studies in CD but treatment is limited by adverse events in high rate and rarely sustainable.
Granulocyte- monocyte apheresis has a limited effect (mainly in UC). Fecal microbial transplantation has emerged a promising treatment with negligible side effects. However, studies using different techniques have yielded limited short-term benefit only.
Autologous hematopoietic stem cell transplant is regarded as a “last resort” option for patients with refractory CD but was studied so far only in adults with promising results though carrying a very high rate of adverse events.
Finally, in the last 2-3 years evidence accumulate on combination of different biologics. Though expensive, such combination may provide relief in refractory cases but more research is needed.
Direct health care costs have shifted towards drug-related expenditures in patients with inflammatory bowel disease (IBD). Frequently, patients will have to switch to a second- or third-line biological therapy due to no response or loss of response. The aim of this study was to describe the use and efficacy of biological therapy in a tertiary centre during a 10-year period and investigate the need for surgery.
The study population consisted of all bio-naïve IBD patients who initiated biological therapy between January 1, 2010 and February 19, 2020 at the Gastro unit, Hvidovre Hospital, Denmark. The electronic medical records were reviewed, and data were systematically registered. Failure of the biological therapy as no response and loss of response was defined by the need for surgery, steroid or shift in biological therapy.
ResultsThe study population consisted of 291 (46.9%) patients with ulcerative colitis (UC), 327 (52.7%) with Crohn’s disease (CD) and 3 with (0.5%) IBD Unclassified (IBDU), who initiated biological therapy with a median follow-up of 3 (IQR=2-5) years from initiation of therapy. The annual number of patients who initiated biological therapy was increasing throughout the study period.
Most patients (457, 73.6%) received one biological drug, 126 (20.3%) received two, and 38 (6.1%) received three or more different types of biological drugs during the study period. Systemic steroid was required in 99 patients (15.9%) and the 5-year surgery-free survival was 76.5% (120 patients with surgery). 302 patients (54.3%) had effect of the first biological therapy at one year follow-up.
In multivariate Cox-regression analyses, concurrent treatment with thiopurines decreased the risk of failure of the first biological therapy in UC patients (hazard ratio (HR) 0.745, 95% CI: 0.559-0.992) but not in CD patients (HR 0.969, 95% CI: 0.722-1.300). Male gender decreased the risk of failure (HR: 0.677, 95% CI: 0.505-0.908) while higher age at initiation of biological therapy increased the risk (HR: 1.0152, 95% CI: 1.004-1.027) in CD patients. These factors had no impact in UC patients. Prior surgery, disease duration and location were not associated with increased risk of failure of first biological therapy.

In conclusion, an increasing number of IBD patients received biological therapy during the 10-year period at our tertiary centre. A considerable part of IBD patients in biological therapy will require surgery, additional steroids, or second line biological therapy. Our findings suggest a beneficial role of thiopurine in combination with biological therapy. Improved identification of patients not responding to first line biological therapy is of great importance.
Learning Objectives:
1. Optimisation, Therapeutic Drug Monitoring of biological
2. Management of anti-drug-antibodies, allergic reaction
3. Strategies PRO / RE-active
Learning Objectives:
1. Acknowledging the risk of cancer in long-standing IBD
2. Surveillance colonoscopy for IBD
3. Managing dysplasia in the IBD setting
4.Surveillance programs and multidisciplinary decision making
5. Surveillance endoscopy
6. Structuring disease, nutrition, endoscopic and surgical options
7. Multidisciplinary decisions
Thinking out of the box. In this talk I will express my personal opinion how surgery can play a role in five year’s time. The role of surgery for IBD moved away from being only a goalkeeper for complicated disease to first line surgery as preparation for medical management or primarily in combination with medical therapy as well.
Examples will be given: Surgery as first line therapy in limited intestinal Crohn’s, surgery in combination with medical therapy for perianal disease aiming at closure, appendicectomy for all or in selected cases, and what the optimal ileocecal resection must be with respect to type of anastomosis and mesenterectomy.
Educational objectives:
1. To understand the metabolism of thiopurines
2. To understand how thiopurine methyltransferase (TPMT) guides thiopurines dosing
3. To have an overview of the role of thiopurine metabolite testing
4. To understand how shunting of thiopurines affects their efficacy and how this can be corrected
This talk will address the use of thiopurines in inflammatory bowel disease. The talk will focus firstly on how pharmacogenetic assessment of patients can improve the risk profile of thiopurine therapy and secondly how therapeutic drug monitoring can also improve the safety as well as maximising the effectiveness of thiopurine use
Intestinal Ultrasound in IBD.
Tip and trick on how to optimise your image
Giovanni Maconi
Intestinal ultrasound (IUS) has become in the last decades an important diagnostic tool for patients with suspected inflammatory bowel diseases (IBD) and for the management and follow up of patients with well-known Crohn’s disease or ulcerative colitis. Thanks to its non-invasiveness and accuracy, the ECCO-ESGAR guidelines recommend IUS as a valuable and practical tool for the assessment of disease activity, monitoring treatment, postoperative recurrence and complications, especially in Crohn's disease (CD).
However, IUS assessment of IBD can be challenging and its accuracy may vary according to targets (e.g. detection, activity, complications), habitus and features of patients, the clinical context, and sonographer experience. The proper use of sonographic machine and adoption of tips and tricks to optimize bowel visualization are leading points to improve diagnostic yield, assess activity and detect complications. Among the relevant steps ,there are the optimization of gain settings, choose the right probe, appropriately set the color Doppler, use appropriately frame rate and other setting devices such as the Pulse Repetition Frequency (PRF). The real time assessment is also crucial, this includes the appropriate use of the graded compression, change of patients position, and use additional techniques such as the oral or intravenous contrast agents. These steps may be very useful to improve the visualization of the bowel, discriminate specific lesions and conditions and overall to improve sonographic assessment of IBD.
Tofacitinib is an oral, small molecule JAK inhibitor for the treatment of ulcerative colitis (UC). Efficacy and safety of tofacitinib were evaluated in randomised, placebo-controlled Phase (P)2 (NCT00787202) and P3 (NCT01465763; NCT01458951; NCT01458574) studies, an open-label, long-term extension (OLE) study (NCT01470612) and an ongoing P3b/4 study (NCT03281304). We report updated tofacitinib safety analyses from the tofacitinib UC clinical programme, with inclusion of a 6‑month interim analysis of data from the P3b/4 study, up to 7.8 years of tofacitinib exposure.
MethodsThis analysis included1157 patients (pts) receiving tofacitinib 5 or 10 mg BID from completed P2/P3/OLE studies, and the ongoing P3b/4 study (as of 20 Feb 2020; Overall+P3b/4 Cohort). Proportions and incidence rates (IRs; unique pts with events/100 pt‑years [PY] of exposure) were evaluated for deaths and adverse events (AEs) of special interest. Opportunistic infections (OIs), malignancies, major adverse cardiovascular events (MACE) and gastrointestinal perforations were adjudicated.
ResultsTable 1 shows demographics and clinical characteristics. In the Overall+P3b/4 Cohort, 1157 pts received ≥1 dose of tofacitinib 5 or 10 mg BID; 955 (83%) received a predominant dose of 10 mg BID; 397/1157 (34.3%) pts had received tofacitinib for >4.1 years. Median treatment duration was 623 (range, 1–2850) days (2999.7 PY of exposure). Table 2 shows safety data for AEs of special interest in the Overall+P3b/4 Cohort. IRs (95% confidence intervals) for all tofacitinib doses: deaths, 0.23 (0.09, 0.46); serious infections, 1.69 (1.26, 2.21); herpes zoster (non-serious and serious), 3.30 (2.67, 4.04); OIs, 1.03 (0.70, 1.46); malignancies (excluding non-melanoma skin cancer [NMSC]), 0.84 (0.55, 1.24); NMSC, 0.73 (0.45, 1.10); MACE, 0.29 (0.13, 0.55); deep vein thrombosis, 0.03 (0.00, 0.18); pulmonary embolism, 0.19 (0.07, 0.42); and gastrointestinal perforations, 0.10 (0.02, 0.28). IRs for AEs of special interest were similar to prior Overall Cohort analyses.1
ConclusionThe safety profile of tofacitinib in pts with UC from the tofacitinib UC clinical programme was generally consistent with that of other UC therapies, including biologics, with the exception of herpes zoster.2 IRs for AEs of special interest have remained stable over an extended period of time (up to 7.8 years) with inclusion of final data from the OLE study and an interim analysis of data from the P3b/4 study.1,3
References:
1. Sandborn WJ et al. United European Gastroenterol J 2021; 9 (Suppl 8): Abstract OP152.
2. Curtis JR et al. Inflamm Bowel Dis 2021; 27: 1394-1408.
3. Sandborn WJ et al. United European Gastroenterol J 2020; 8 (Suppl 8): Abstract OP494.

Paediatric Inflammatory Bowel Disease (IBD) accounts for 10-15% of all incident cases, while incidence in children under 10 years old is rising most rapidly. Very early-onset inflammatory bowel disease (VEOIBD) is diagnosed before the age of 6 years while infantile IBD occurs before the age of 2 years and may be a clue for monogenic IBD..
It is very important to identify monogenic IBD patients as management may differ from classical IBD. While age of onset is most relevant, specific comorbidity and extraintestinal manifestations also are of particular relevance in identification of monogenic IBD. These conditions are summarized in the following: Young agematters most. Young age onset; Multiple family members and consanguinity; Autoimmunity; Thriving failure; Treatment with conventional medication fails; Endocrine concerns; Recurrent infections or unexplained fever; Severe perianal disease; Macrophage activation syndrome and HLH; Obstruction and atresia of intestine; Skin lesions, dental and hair abnormalities; Tumours. This anagram will be further elucidated.
A diagnostic algorithm of monogenic IBD will be discussed, incorporating multidisciplinary team assessment of genetic results, genetic counselling but also the need for functional assessment of novel gene defects and variants of unknown significance to establish causality. Also, illustrative cases of monogenic IBD such as Interleukin-10 receptor deficiency and XIAP will be incorporated in the presentation.
Disease location is a prominent axis of heterogeneity in Inflammatory Bowel Disease (IBD) with many implications. Using genome-wide profiling of the transcriptome of monocytes and CD4+ T cells isolated and purified from whole blood, we aimed to identify molecular signatures and mechanisms associated with different locations among IBD patients.
Blood was collected from 125 IBD patients (87 CD, 38 UC) with endoscopy-proven active disease (presence of ulcerations). Cell separation and fluorescence activated cell sorting were performed to separate the monocyte and CD4+ T cell fractions, from which RNA was subsequently isolated and sequenced (Illumina HiSeq 4000NGS). We used different supervised and unsupervised approaches (differential expression, pathway based data integration, latent factor based models, regularized generalized canonical correlation analysis and co-expression networks) to interpret the differences in the gene expression datasets of monocytes and CD4+ T cells from patients with different disease locations (Montreal classification). Functional enrichment analysis was performed using the ReactomePA package. Regulatory relationships and therapeutic relevance information were retrieved from the ChEA3 and the OpenTargets resources respectively. Comparison with single-cell and bulk-derived gene expression signatures from other auto-immune diseases were performed using the ADEX resource.
ResultsHighly variant disease-location (DL)-associated genes (FDR <= 0.1) in monocytes and CD4+ T cells were identified using latent factor based unsupervised models. These genes were known to be involved in IBD pathogenesis and/or intestinal inflammation. Additional supervised analysis revealed significant differences in CD4+ T cells between ileal CD patients and UC patients. RAF-independent MAPK-activation pathway and FOXO-mediated transcriptional pathway (downregulated in UC patients) were over-represented (FDR <= 0.05) among the features distinguishing ileal CD and UC patients based on signature sets derived from the above-mentioned multiple approaches. Of note was the finding that 12.5% of the DL associated co-expression modules were also annotated as IBD drug targets. Based on gene expression signature from bulk and single-cell sources, the DL associated genes were found to be active in many other auto-immune diseases such as rheumatoid arthritis, systemic sclerosis, Sjögren’s syndrome, type 1 diabetes and Systemic lupus erythematosus, suggesting their role in mediating immune malfunctions.
ConclusionWe identified signaling pathways and transcription factors which could drive the expression differences observed in the circulating immune cells between ileal CD and UC patients.
Educational objectives
How to define endoscopic remission (ER) and transmural remission (TR) in Crohn’s disease
PROS and CONS for endoscopic remission in CD
PROS and CONS for transmural remission in CD
Potential algorithm on how and when to assess ER and TR as potential treatment target in CDSubcutaneous (SC) formulations of CT-P13 and vedolizumab (VED) are currently available as new treatment option for patients with inflammatory bowel disease (IBD). The decision to switch requires a shared decision making based on adequate education of the patient, to avoid negative outcomes due to a nocebo effect. The aims of this study were (1) to evaluate the percentage of patients with IBD in favour of switching to SC formulations and (2) to compare two educational strategies.
MethodsThis was a multicentre study in patients with IBD on maintenance intravenous (IV) CT-P13 or VED. Patients attending the infusion unit were invited to complete a survey exploring the willingness to switch to SC formulations. In centre A, all patients were informed on the new SC formulations and the accompanying care pathway by an information leaflet and a face-to-face interaction with the IBD nurse, prior to completing the survey. In centre B, patients on a minimal interval of q8w were digital invited to the same survey via the e-health application of the hospital. Demographics, patient reported outcomes, willingness to switch and reasons for IV vs. SC preferences were captured.
ResultsIn total, 447 (n=183 Centre A; n=264 Centre B; participation ratio 83.6%) patients completed the survey (m/f: 212/235; CD/UC/IBD-U: 275/161/11; median age 45 IQR 33-57; remission CD/UC: 75%/82%) see table. Most patients were open to SC treatment (47% yes, 33% doubt, 20% no). The main driver to switch was an anticipated decrease in hospital visits (86%) and overall time gain (78%). The main reason to continue IV was fear of change (60%) and uncertainty in case of relapse after switch to a SC formulation (46%). In univariate analysis, the self-estimated compliance rate was associated with the willingness to switch (p<0.0001). To evaluate the impact of the approach in patient education between the two centres, we compared the subgroup of patients on ≥q8w interval with a dosing of 5-10mg/kg CT-P13 or 300 mg VED (n=335). The willingness to switch was higher after a face-to-face approach (centre A) compared to a merely digital approach (centre B; 53.9 % vs. 40.9 % p=0.038), although patients in centre B had a higher educational level (p=0.003), more prior experience with other IBD SC medication (p=<0.001), lived further from the hospital (p<0.001) and had a younger age at diagnosis (p=0.019).
ConclusionIn this multicentre comparative study exploring the willingness to switch from IV to SC maintenance therapy with CT-P13 and VED, the majority is open to switch to a SC formulation. The direct approach and education of the patient by the IBD nurse impacts significantly the willingness to switch. In a follow-up we will investigate the actual switch rates.
1. To review flare management and optimisation of biologic treatments using TDM
2. To choose an appropriate therapy for pregnant IBD patients
3. To learn how to plan peri-partum care
1. To review the therapeutic goals and patient needs in UC
2. To confer different treatment strategies in UC
3. To discuss therapeutic options in UC
4. To emphasize the advantage of tight disease control
We sought out to identify proteomic markers of anti-Tumor Necrosis Factor (TNF) treatment failure in anti-TNF naive patients with Crohn's disease, using data obtained from the Personalised Anti-TNF Therapy in Crohn's disease (PANTS) study.
Background
The first line treatment for inducing remission in pediatric Crohn’s disease (CD) is Exclusive Enteral Nutrition (EEN), where a patient drinks a nutritionally complete formula exclusively for 6 to 12 weeks. Despite the effectiveness of EEN, some patients may experience challenges including taste fatigue, monotony, and a lack of social participation with meals. Given these challenges, patients may turn to popular or fad diets for managing their disease. These diets are often restrictive, eliminating a number of foods and exacerbating the risk of underlying nutrient deficiencies in this patient population.
Methods
These case studies involved a nutrient analysis of evidence-based and popular diets for CD, including Crohn’s Disease Exclusion Diet (CDED), CD-TREAT, Specific Carbohydrate Diet (SCD), IBD Anti-inflammatory Diet (IBD-AID), Autoimmune Protocol (AIP) Diet, Gut and Psychology Syndrome (GAPS) Diet, and low FODMAP. Four cases were selected with mild-moderate CD: 11-year-old and 16-year-old, both male and female. A nutrient analysis of sample menus of each diet was completed using Food Processor version of 11.6.0 by ESHA Research. Results were compared to age and gender specific Dietary Reference Intakes (DRIs), population-based dietary intake data, and Health Canada Dietary Guidelines.
Results
Data are presented for Case 1, 11-year-old male. Findings were comparable to other age and gender cases. As compared to Acceptable Macronutrient Distribution Ranges (AMDRs), there was a higher percentage of energy from fats and lower from carbohydrates for the SCD (% kcal, fat and carbohydrate respectively: 59%; 30%), IBD-AID (52%; 37%), AIP Diet (50%; 20%) and GAPS Diet (60%, 21%). Saturated fat intake exceeded recommendations (>10% of energy intake) for CDED (% kcal, 14%) CD Treat (17%), SCD (11%), AIP Diet (15%) and GAPS Diet (20%). Both vitamin D and/or calcium intake were below the Recommended Dietary Allowance (RDA) respectively for CDED (% RDA, vitamin D and calcium respectively: 89%; 86%), SCD (23%; 53%), AIP Diet (14%; 23%), low FODMAP Diet (4%, 96%) and GAPS Diet (calcium, 58%). Adolescent females versus males between the ages of 14-18 years may be at greater risk of inadequate nutrient intake, given the general increase in nutrient requirements yet lower caloric needs.
Conclusion
Given the increase in awareness and interest in popular diets for Crohn’s disease, it is imperative that clinicians are aware of the risks of inadequate nutrient intake with restrictive diets.


