Pouchitis is a common complication of ileal pouch-anal anastomosis (IPAA) after proctocolectomy in ulcerative colitis (UC). There are currently no approved therapies for chronic pouchitis. Here, we report a multicentre trial of intravenous (IV) vedolizumab (VDZ) for chronic pouchitis after IPAA in patients with UC.
MethodsEARNEST was a randomised, double-blind, placebo (PBO)-controlled, phase 4 study of VDZ in patients aged 18-80 years with chronic pouchitis after proctocolectomy with IPAA for UC (NCT02790138). Male and female patients with a history of IPAA for UC and chronic pouchitis were eligible. Patients were randomised (1:1) to receive VDZ IV (300 mg) or PBO on Day 1 and at Weeks (W) 2, 6, 14, 22 and 30, as well as ciprofloxacin for the first 4 weeks. The primary endpoint was modified Pouchitis Disease Activity Index (mPDAI) remission at W14; efficacy was also assessed through other mPDAI/PDAI secondary endpoints and endoscopic exploratory endpoints (assessed by a central reviewer) at W14 and W34. Safety (adverse events [AEs]) was monitored throughout the study.
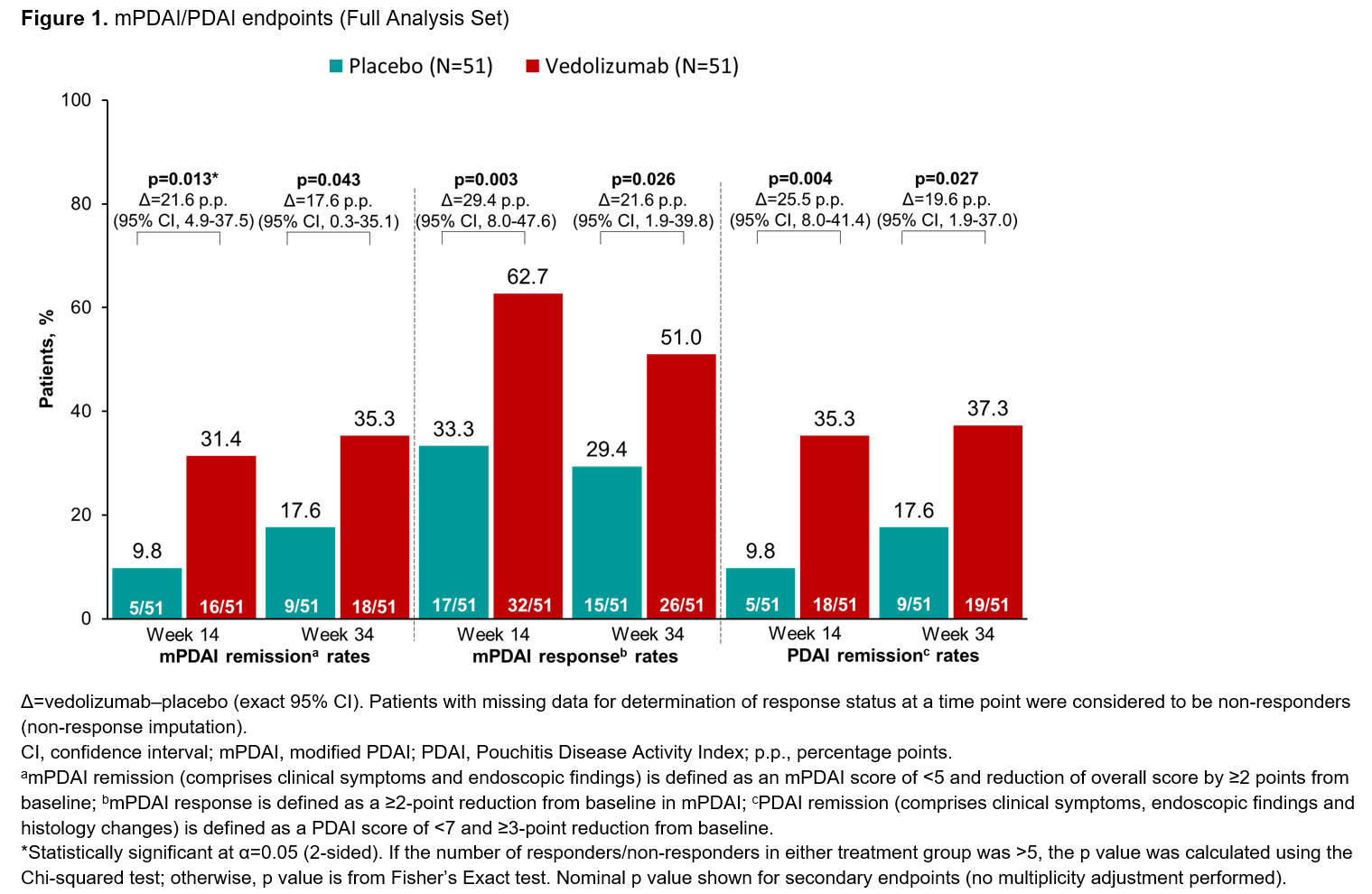
ResultsIn total, 102 patients were treated (51 per group). Patients had a mean age of 40.8 years (VDZ) and 42.9 years (PBO). mPDAI remission rates (comprising clinical symptoms and endoscopy domains) were 31.4% (n=16/51) for VDZ vs 9.8% (n=5/51) for PBO at W14 (p=0.013; Figure 1). Significant differences in favour of VDZ over PBO were also seen in mPDAI remission at W34, mPDAI response at W14 and W34, and PDAI remission (comprising clinical symptoms, endoscopy and histology domains) at W14 and W34 (Figure 1). The rate of sustained remission (defined as remission at both W14 and W34) was higher for VDZ vs PBO on both the mPDAI (VDZ 27.5% [n=14/51] vs PBO 5.9% [n=3/51]; difference 21.6 percentage points [95% confidence interval (CI), 6.5-37.0]) and the PDAI (VDZ 31.4% [n=16/51] vs PBO 7.8% [4/51]; difference 23.5 percentage points [95% CI, 8.0-38.8]). Endoscopic ulceration analysis showed greater reductions in number of ulcers from baseline for VDZ over PBO at W14 and W34 (Figure 2). A higher proportion of patients in the VDZ vs PBO group had an improved SES-CD score and achieved SES-CD remission of pouchitis (Figure 2). AE rates were similar between groups and no new safety signals were identified (Table).
 Conclusion
ConclusionThis is the first and largest randomised, double-blind PBO-controlled trial of biologic therapy to show significant benefits across multiple treatment outcomes in patients with chronic pouchitis after IPAA for UC. VDZ showed consistent treatment benefits over PBO across clinical, endoscopic and histologic endpoints, together with safety consistent with its established profile.
Patients admitted to hospital with active Inflammatory bowel disease(IBD) are at increased risk of thromboembolism. Surgical specialties have demonstrated benefits of thromboembolism prophylaxis after hospital discharge in high risk groups.
This study aims to identify IBD patients at increased risk and develop a scoring system to recognise them.
MethodsHospital episode statistics data was used to identify all patients admitted for IBD emergently or electively for surgery. All Patients with a thromboembolism within 90 days of hospital discharge were identified. A multilevel logistic regression model was used to identify patient and admission level factors associated with increased risk of thromboembolism. A scoring system to identify higher risk patients was constructed based on this model. Score performance was assessed using bootstrapped data.
Results201,779 admissions in 101,966 patients were included. The rate of thromboembolism within 90 days was 17.24 per 1000 patient years at risk. This was highest in patients admitted as an emergency undergoing surgery (36.91) followed by emergency admission without surgery (15.63) and elective admission for surgery (15.60). The rate of thromboembolism between 180 and 270 days following discharge was 0.84, 1.59 and 1.70 per 1000 patient years at risk respectively.
Regression analysis demonstrated that female gender (OR 0.65(95%CI 0.53-0.80),p<0.001), increasing age (49-60 years,(4.73(3.40-6.58),p<0.001), increasing length of stay; 5-7 days (1.77(1.27-2.46),p=0.001), 7-10 days (1.91(1.40-2.60),p<0.001), >10 days (4.04(2.98-5.46),p<0.001), increasing number of prior admissions for IBD in preceding 3 months; 1 (1.36(1.11-1.68),p=0.004), 2 (1.66(1.23-2.22),p=0.001), >2 (2.32(1.67-3.21),p<0.001), Ulcerative Colitis (1.46(1.19-1.79),p<0.001) and admission type compared to Elective surgery (Emergency admission including surgery (1.64(1.15-2.33),p=0.006)), (Emergency admission not including surgery(1.57(1.07-2.32), p=0.023)) were statistically significant associations.
In the scoring system, a score >=9 gave a positive predictive value of 1%. The AUC was 0.71(95%CI 0.69-0.72)
ConclusionPatients admitted to hospital have ongoing increased risk of thromboembolism in the 90 day period following discharge. Risk was increased in patients with prolonged length of stay, increasing age, male gender or admitted as an emergency requiring surgery. Higher risk patients were identifiable by a scoring system.
An overview of wearable and remote technology for monitoring of IBD
Objectives:
1. To link between changes in IBD incidence rates and changes in lifestyle habits around the world
2. To demonstrate the global association between ultra-processed food intake and IBD risk
3. To review the literature focusing on the Mediterranean diet and IBD across the globe
What is the optimal timing and methods for monitoring?
Educational objectives:
1. To understand the importance of disease monitoring in a treat-to-target strategy
2. To understand the difference between a treatment target and an instrument of tight disease control
3. To understand the need for a non invasive patient-friendly disease monitoring
4. To emphasize a proposal for a structured time-bound monitoring
Disease monitoring is the corner-stone of a treat-to-target strategy. The definition of the treatment target is linked to our understanding of the disease process and the availability of markers to assess the disease process. Beside the target, we may define several steps to reach the target which are associated with specific tools and markers. Monitoring tools are not unique and must be articulated in a time-bound manner to allow an optimal disease control aiming at alleviating the symptoms and avoiding disease progression. In particular is a full endoscopic healing is currently the most widely accepted objective, intermediate steps may include symptomatic improvement and biomarkers improvement and normalization.
Up to 50% of Crohn’s patients develop intestinal strictures during their disease course. In general, predominant-inflammatory strictures are likely to benefit from anti-inflammatory medical therapy, whereas predominant-fibrotic strictures often require endoscopical/surgical approach. However, rarely is a stricture merely inflammatory or fibrotic; they are typically characterised by a mixture of inflammation, muscular hypertrophy, collagen disposition and fibrosis. Cross-sectional imaging techniques allow full-thickness evaluation of the bowel wall, of which IUS is non-invasive, cost-effective and can be used in the point-of-care setting, which makes is an attractive tool for monitoring.
The aim of the talk is to review the challenges of distinguishing inflammatory and non-inflammation strictures on conventional B-mode IUS and on advanced US modalities, such as CEUS and elastography.
To understand imaging findigs of Fibrosis on cross sectional imaging with emphasis on MR-E
To review litterature on MR-E and fibrosis
To have an overview over new imaging tools of Fibrosis (delayed enhancement, DWI, IVIM, Magnetization trasfert, Motility study).
Educational Objectives:
1. To appreciate the strong impact of the diet on gut microbial community structure and function
2. To understand the role of the diet in the pathogenesis of experimental gut inflammation
3. To review a role of the diet on the development and course of human inflammatory bowel diseases
1) Overview of the aetiology of IBD
2) Discussion of the impact of the environment on disease onset, course and response to therapy
3) Focus on the emerging evidence of a role of diet on disease onset from animal models, epidemiology and human studies
4) Discussion of the potential to modify the environment as a preventative strategy / therapy
Learning Objectives:
1. Screening before immunosuppression and immunisation
2. Indications for biological therapy
3. Evaluation of response
IBD patients are eligible to treatment with biologic agents if they have failed or cannot tolerate conventional treatment with corticosteroids and/or immunomodulators (IMMs) or are corticosteroid dependent. Early introduction of biologic therapy is also recommended for patients who at diagnosis have clinical features that predict a disabling course of disease. Ideally, patients should be screened for infectious diseases, malignancies, and complete all essential vaccinations before starting any therapy. Selecting the best biologic amongst the currently available different classes, depends on several patient- and disease-related parameters, such as age, disease activity, comorbidities, and the overall burden of disease. As for any therapy, it is important to define short-, medium- and long-term goals, monitor the progress of disease and adapt treatment accordingly (treat to target).
The first biologic is the best shot. Thus, it is key to adapt dosing to disease activity to avoid primary non-response or partial response and thus achieve a better long-term response. Co-treatment with an IMM may influence the pharmacokinetics in particular of anti-TNF and prevent early development of anti-drug antibodies ADA). Once clinical remission has been achieved, patients should be closely followed by monitoring clinical activity (patient reported outcomes), biomarkers (serum CRP, faecal calprotectin), imaging (US, MRE), endoscopy and/or histology. Treatment optimization in case patient loses response can be achieved either empirically (Standard of Care) by increasing the dose of the biologic or halving the administration interval, or both, or by adding an IMM, or by therapeutic drug monitoring (TDM), i.e., by measuring drug levels and ADA. Pro-active TDM has not been proven superior to reactive TDM, still, it serves to discriminate between pharmacokinetic and pharmacodynamic failure of treatment. However, proactive TDM is increasingly used to achieve clinical response and/or remission during induction, to de-escalate, or stop biologic therapy.
4. Screening before immunosuppression and immunisation
5. Indications for biological therapy
6. Evaluation of response
Educational objectives:
1. To understand growth impairment in paediatric IBD resulting from disease activity & treatment choices
2. To review the current ECCO/ESPGHAN treatment algorithm with regards to growth optimization
3. To provide an overview of strategies to minimize IBD activity-related growth impairment
4. To emphasise the importance of reducing steroid-exposure and improving skeletal growth and lean body mass
- understand approaches of using Omics-based medicine in other disciplines (oncology)
- review current mainstays in OMICS-based diagnostics
- get an overview of current trial designs on implementing omics into patient care
Combination therapy with infliximab and anti-metabolites is a standard option for patients with Crohn’s disease (CD). The implications of long term use of combination therapy may lead patients and clinicians to contemplate treatment de-escalation once steroid-free remission has been achieved. The aim of our study was to assess the relapse rates and time spent in remission over 2 years, after withdrawal of infliximab or anti-metabolite compared to continuation of combination therapy.
MethodsCD patients treated with a combination therapy of infliximab (IFX) and anti-metabolite > 8 months and in sustained steroid-free remission > 6 months were recruited in 64 centers in France, United Kingdom, Belgium, Sweden, Australia, Germany and The Netherlands. Patients were randomized into 3 arms - continuing combination therapy (arm A); stopping IFX (arm B); or stopping anti-metabolite (arm C). In case of a relapse [defined by CDAI and an objective marker of inflammation (CRP or fecal calprotectin)], patients were retreated by resuming infliximab in arm B or the anti-metabolite in arm C, according to a pre-defined scheme, including optimization of IFX up to 10 mg/Kg if necessary in all arms. The two co-primary endpoints were the relapse rate and mean survival time spent in remission over 2 years. A major secondary endpoint was treatment failure (complications or not recapturing remission).
Results254 patients were screened, 211 randomized, 5 withdrew consent and 1 was lost to follow-up, leaving 205 patients for the analysis - 67 randomized to arm A, 71 to arm B and 67 to arm C. Demographic and clinical characteristics are shown in Table 1. The two-year relapse rates were 14% (IC95%: 4-23%) in arm A, 40% (IC95%: 28-51%) in arm B, and 10% (IC95%: 2-18%) in arm C (p=0.0003 arm B vs arm A and <0.0001 arm B vs arm C) (figure 1). The time spent in remission was 1.91 yrs (IC95%: 1.83-1.99), 1.89 yrs (IC95%: 1.82-1.96) and 1.93 yrs (IC95%: 1.86-2.00) in arm A, B and C, respectively. Out of the 39 relapsers, 28 were retreated/optimized. Remission was achieved in 1/2 retreated patients in arm A, 22/23 in arm B and 2/3 in arm C. Treatment failure was observed in 4/67, 4/71 and 3/67 patients, in these three arms, respectively. No malignancy was observed, one tuberculosis in arm C and two severe infections (pneumonia and viral pericarditis) in arm B.
ConclusionInfliximab withdrawal, but not antimetabolite withdrawal, was associated with a significantly higher risk of relapse than continuation of combination therapy. Almost all patients who stopped IFX achieved rapid remission when resuming treatment. The time spent in remission over 2 years was similar across groups.
1. To outline the multifactorial etiology of perianal CD
2. To describe advances in diagnosis in perianal CD over the last 10 years
3. To detail advances in medical and surgical therapy in perianal CD over the last decade
4. To understand the different therapeutic options for future management of perianal CD
1) To have an overview of the recent advances in surgery for ulcerative colitis
2) To understand the benefits of the laparoscopic approach for surgery in UC patients
3) to review the possible alternatives to pouch surgery in patients with UC: ileorectal anastomosis, appendectomy, ileostomy, segmental colectomy
Educational objectives:
1. To understand the role of 5-ASA in the treatment of IBD and the most frequent mistakes made in 5-ASA treatment
2. To review the evidence for dosing and treatment routes for the different localizations of inflammation in UC and CD
3. To emphasise the role of rectal 5-ASA therapy in proctitis and left sided colitis and the important role of oral/rectal combination therapy
4. To have an overview over optimal treatment strategies with 5-ASA
Organoids are self-renewing, 3D structures, consisting of different cell types, with histology and physiology features very close to the physiology of the studied organ. Specifically, human Intestinal Organoids (HIOs) develop epithelial crypts consisting of all subtypes of intestinal epithelial cells which are surrounded by mesenchymal cells. Our aim was to develop 3D HIOs from human embryonic stem cells (hESCs) and examine the expression of fibrotic and mesenchymal factors during their maturation process. Additionally, we investigated the effect of the pro-inflammatory cytokines, IL-1α and TNF-α on the expression of fibrotic and inflammatory mediators in HIOs.
MethodsThe human ESC line (H1) was cultured and then differentiated towards HIOs using commercially available kit. HIOs were characterized by immunofluorescence in all differentiation stages. In order to examine their maturation process, we compared the mRNA expression of fibrotic and mesenchymal markers from passages 1-10. In order to examine their functionality, HIOs from different passages were stimulated with 5ng/ml IL-1α and 50ng/ml TNF-α for 12 hours, total RNA was collected and the fibrotic and inflammatory mRNA expression was examined. The mRNA transcripts of CD90, collagen type I, III, fibronectin, CXCL8, CXCL10 and CXCL11 were measured by reverse transcription quantitative PCR.
ResultsHIOs were successfully developed as they were stained positive for all tested markers throughout their developmental process. Regarding their maturation process, we observed high expression of CD90, collagen type I, type III and fibronectin that was gradually decreased during passages. As for the fibrotic and inflammatory responses from HIOs, we found that the IL-1α and TNF-α stimulation resulted in statistically significant upregulation of the fibrotic factors, fibronectin, collagen type I and type III in culture passages 2 and 4, but had no effect in culture passages 8 and 10. Similarly, IL-1α and TNF-α stimulation led to the statistically significant induction of the inflammatory chemokines CXCL8, CXCL10 and CXCL11 in culture passages 2 and 4, while no effect was observed in culture passages 8 and 10.
ConclusionOur findings indicate that HIOs contain a functional mesenchymal component that is gradually diminished during passages. Inflammatory and fibrotic responses of HIOs seem to depend on the fitness of their mesenchyme. IBD studies using HIOs as in vitro models should be performed on early passages, when HIO’s mesenchymal component is still functional.