Very early-onset inflammatory bowel disease (VEOIBD) is diagnosed before the age of 6 years while infantile IBD occurs before the age of 2 years. We aimed to assess disease characteristics and long-term outcomes in these populations.
MethodsWe conducted a retrospective longitudinal cohort study in 21 pediatric centers worldwide. Patients diagnosed with VEOIBD between the years 2008-2018 with at least 2 years of follow-up were included.
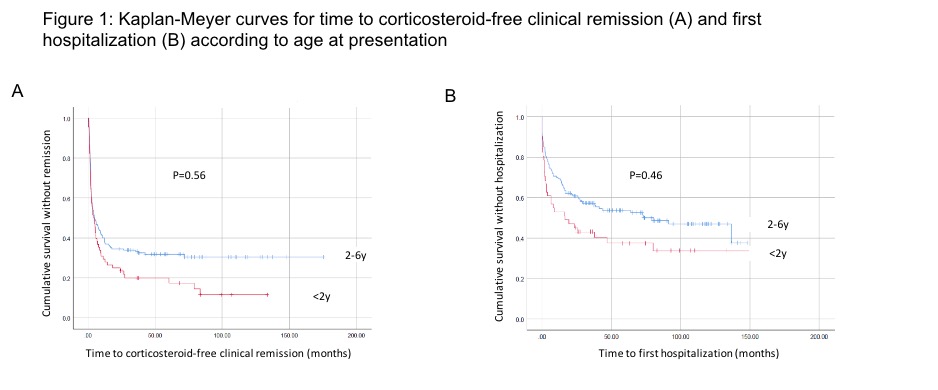
ResultsThe cohort included 243 patients (52% males), with median follow-up of 5.8 (IQR 3.2-8.4) years. Median age at diagnosis was 3.3 (IQR 1.8-4.5) years, with 69 (28%) diagnosed before the age of 2 years. Disease was classified as Crohn’s disease (CD), ulcerative colitis (UC) and IBD-unclassified (IBDU) in 30%, 59% and 11%, respectively. In patients with UC or IBDU, 75% presented with pancolitis. In patients with CD, 62% presented with isolated colonic disease and 32% with ileo-colonic disease, while 19% had perianal involvement. Genetic testing was performed in 96 (40%) patients [40 (58%) <2 years, 56 (32%) 2-6 years, p=0.001], with monogenic diagnosis identified in 23% (33% and 16%, respectively, p=0.08). The most common findings were mutations in IL10-receptor (5 cases, 23%). Stricturing or penetrating disease was observed in 9 cases (4%).
First induction therapies were corticosteroids, 5-aminosalicylic acid (5ASA) and nutritional therapy in 53%, 30% and 11%, respectively. Corticosteroids were more common as first induction in infantile vs. non-infantile IBD (64% vs. 49% respectively, p=0.003). Maintenance therapies included deep immune-suppression (mainly biologics and corticosteroids) in 51%, immunomodulators in 27%, and non-immunosuppressive agents (5-ASA, nutritional therapy and antibiotics) in 22% of patients, with no significant differences between age groups.
Compared to patients diagnosed after 2 years of age, patients with infantile IBD presented with higher rates of IBDU, lower levels of hemoglobin and albumin and higher levels of CRP, lower weight (but not height) z-scores, had lower rates of response to first induction therapy and shorter time to hospitalization during follow-up (p<0.05 for all).
Colectomy was performed in 11% and diversion surgery in 4% of the cohort, with no significant differences between age groups. No malignancies and nor deaths were observed. At end of follow-up, 85% of patients were in corticosteroid free clinical remission.
 Conclusion
ConclusionPatients with VEOIBD, including infantile IBD, have fair long-term outcome with low rates of complications and surgical interventions. Nevertheless, patients with infantile IBD demonstrated more severe clinical features at presentation and a lower response to induction therapy.
In the UNIFI study of ustekinumab (UST) in ulcerative colitis (UC), patients who achieved histo-endoscopic mucosal healing (HEMH; ie, both histologic and endoscopic improvement of mucosa) after induction had higher clinical remission and corticosteroid-free clinical remission rates through 1 year than those who achieved either histologic or endoscopic improvement alone.1 Here, we report the effect of achieving HEMH after induction on long-term symptomatic outcomes through 3 years.
MethodsPatients who were in clinical response after 8 wks of IV induction with UST 130mg or ~6mg/kg (wk 8 responders) were randomized to maintenance treatment with SC UST 90mg q12w or q8w on entry into maintenance. Those who were not in clinical response to the initial UST dose at wk8 but achieved response at wk16 after receiving a single SC dose of UST 90mg at wk8 (wk16 responders) entered maintenance receiving SC 90mg q8w. After 44 wks of maintenance treatment, patients were given the option to continue in the long-term extension. HEMH was defined as achieving both endoscopic improvement (Mayo endoscopy subscore ≤1) and histologic improvement (neutrophil infiltration in <5% of crypts, no crypt destruction, and no erosions, ulcerations, or granulation tissue; based on the Geboes score). Patients with insufficient data for histologic evaluation at the end of induction were excluded. Symptomatic remission was defined as a Mayo stool frequency subscore of 0 or 1 and a Mayo rectal bleeding subscore of 0.
ResultsOf the 438 patients who were wk8 or wk16 responders to UST induction and received UST maintenance, 116 (26.5%) achieved HEMH after induction, 30 (6.8%) achieved endoscopic improvement without histologic improvement (EI), and 106 (24.2%) achieved histologic improvement without endoscopic improvement (HI). Patients who achieved HEMH after induction had higher symptomatic remission and corticosteroid-free symptomatic remission rates at wks92 and 152 than those with EI or HI; the differences were statistically significantly greater at wk152, while they were only numerically greater at wk92 (Table). The differences were primarily driven by patients with HEMH after induction being more likely to maintain symptomatic remission between wks92 and 152, than those with EI or HI alone. Symptomatic remission and corticosteroid-free remission rates decreased between wks92 and 152 in patients with EI or HI only.
Patients with UC who achieved HEMH after induction with UST were more likely to maintain symptomatic remission and corticosteroid-free symptomatic remission between 2 and 3 years of maintenance treatment than those who achieved EI or HI alone.
1. K Li, et al. Poster 1008. Presented at UEGW 2019. October 22, 2019. Barcelona, Spain.
The PISA-II trial showed that anti-TNF induction combined with surgical closure induces MRI healing more frequently than anti-TNF alone at 18 months follow-up (FU) and that this was associated with no recurrences at the time. The aim of this study was to compare long-term outcomes of both treatment arms.
MethodsIn this FU study, data were collected from patients who participated in the PISA-II trial, a multicentre, international patient preference randomised controlled trial that compared anti-TNF induction combined with surgical closure to anti-TNF therapy alone as treatment for Crohn’s perianal fistulas. FU data were collected from the time of enrolment in the PISA-II trial until November 2021. Primary outcome was radiological healing at MRI and secondary outcomes included long-term clinical closure, recurrences, anti-TNF trough levels (suboptimal level was defined as infliximab <5.0ug/ml, adalimumab <5.9ug/ml), incontinence (improved, decreased or never had), and a decisional regret scale.
ResultsLong-term FU data were collected from 88 out of 94 patients included in the PISA-II trial, 35/38 in the surgical closure arm and 53/56 in the anti-TNF treatment arm. Median FU was 5 years (IQR 4-7). During long-term FU radiological healing occurred in significantly more patients in the surgical closure arm (40% vs 17%; P=0.018). Long-term clinical closure occurred in 71% in the surgical closure arm and in 60% in the anti-TNF treatment arm (P=0.533). Recurrences occurred in 20% in the surgical closure arm and in 36% in the anti-TNF treatment arm (P=0.111). One patient with radiological healing developed a recurrence (4.3%) vs 12/57 (21.1%) patients with clinical closure. Trough levels were available in 32/53 patients treated with anti-TNF. Around the time of recurrence a suboptimal anti-TNF serum trough level occurred in 6/10. In the surgical closure arm, 6 patients had more and 6 patients had less incontinence problems after treatment, comparable to the 5 patient in the anti-TNF treatment arm with more and 8 with less incontinence problems. All patients in the surgical closure arm who completed the questionnaire (strongly) agreed that undergoing surgery was the right decision and 79% of the patients in the anti-TNF arm (strongly) agreed, 14% neither agreed nor disagreed and 7% disagreed that anti-TNF treatment was the right decision.
This study further supports the previous finding that anti-TNF induction combined with surgical closure should be considered in patients with Crohn’s perianal fistulas as long-term outcomes are favourable. Interestingly, surgical closure does not seem to be correlated to decreased continence, and all patients agreed that surgery was the right decision.
The PISA-II trial showed that anti-TNF induction combined with surgical closure induces MRI healing more frequently than anti-TNF alone at 18 months follow-up (FU) and that this was associated with no recurrences at the time. The aim of this study was to compare long-term outcomes of both treatment arms.
MethodsIn this FU study, data were collected from patients who participated in the PISA-II trial, a multicentre, international patient preference randomised controlled trial that compared anti-TNF induction combined with surgical closure to anti-TNF therapy alone as treatment for Crohn’s perianal fistulas. FU data were collected from the time of enrolment in the PISA-II trial until November 2021. Primary outcome was radiological healing at MRI and secondary outcomes included long-term clinical closure, recurrences, anti-TNF trough levels (suboptimal level was defined as infliximab <5.0ug/ml, adalimumab <5.9ug/ml), incontinence (improved, decreased or never had), and a decisional regret scale.
ResultsLong-term FU data were collected from 88 out of 94 patients included in the PISA-II trial, 35/38 in the surgical closure arm and 53/56 in the anti-TNF treatment arm. Median FU was 5 years (IQR 4-7). During long-term FU radiological healing occurred in significantly more patients in the surgical closure arm (40% vs 17%; P=0.018). Long-term clinical closure occurred in 71% in the surgical closure arm and in 60% in the anti-TNF treatment arm (P=0.533). Recurrences occurred in 20% in the surgical closure arm and in 36% in the anti-TNF treatment arm (P=0.111). One patient with radiological healing developed a recurrence (4.3%) vs 12/57 (21.1%) patients with clinical closure. Trough levels were available in 32/53 patients treated with anti-TNF. Around the time of recurrence a suboptimal anti-TNF serum trough level occurred in 6/10. In the surgical closure arm, 6 patients had more and 6 patients had less incontinence problems after treatment, comparable to the 5 patient in the anti-TNF treatment arm with more and 8 with less incontinence problems. All patients in the surgical closure arm who completed the questionnaire (strongly) agreed that undergoing surgery was the right decision and 79% of the patients in the anti-TNF arm (strongly) agreed, 14% neither agreed nor disagreed and 7% disagreed that anti-TNF treatment was the right decision.
This study further supports the previous finding that anti-TNF induction combined with surgical closure should be considered in patients with Crohn’s perianal fistulas as long-term outcomes are favourable. Interestingly, surgical closure does not seem to be correlated to decreased continence, and all patients agreed that surgery was the right decision.
Ustekinumab (UST), an anti-interleukin-12/23 antibody, has successfully been introduced in the treatment of IBD, mainly in patients failing anti-TNF-agents. The STOCUSTE study includes IBD patients treated with UST at four teaching hospitals in Stockholm to provide long-term follow-up data. Here, we report the outcome in Crohn’s disease over the first 12 months.
MethodsThis retrospective study includes patients diagnosed with Crohn’s disease and treated with UST who were followed until withdrawal of treatment for any reason, or until end of study, July 31, 2021. Disease activity (Harvey-Bradshaw Index (HBI); Physician Global Assessment (PGA), laboratory parameters and drug persistence were assessed. The primary outcome was remission (HBI ≤4; PGA = 0) and response (decrease HBI ≥3; PGA ≥1 from baseline) at 3 and 12 months, respectively.
Results120 patients, 61 women (51%), with a median age of 27 (IQR 27) at start of UST were included. All patients had luminal disease and 19 (16%) also fistulizing disease. 109 (91%) had failed ≥1 and 59 (49%) ≥2 anti-TNF drugs. In addition, 50 patients (42%) failed vedolizumab. At inclusion, 106 (88%) had active disease; 40 (33%) were on corticosteroid treatment and 22 (18%) on thiopurines.
The persistence on UST was high, 93% at 3 months and 56% at 12 months. Of patients on UST at 3 months, 38% were in remission, and, at 12 months, 53%. An additional 26% were in response at 12 months. Of the 40 patients initially on corticosteroids, 17 (43%) and 28 (70%) had stopped steroids at 3 and 12 months, respectively. The median faecal calprotectin level declined from 272 (90-1763) at baseline to 75 (49-99) µg/g at 3 months (p<0.01). There was a slight decrease in CRP over 12 months, from 3 (2-12) to 1 (1-2) mg/l, together with increases in haemoglobin and serum albumin (n.s).
Withdrawal from treatment during the first 12 months was 44% (53/120), mainly due to persisting disease activity. Four patients were withdrawn due to adverse events, three needed bowel surgery, two had malignancy and one patient suffered from systemic infection.
In this group of difficult-to-treat patients with Crohn’s disease, UST was shown to be effective in the majority, with high drug persistence at 12 months in combination with a favorable safety profile.
Ozanimod was approved by the FDA to treat patients (pts) with moderately to severely active Ulcerative Colitis (UC) based on the results from the 52-week (wk) phase 3 True North (TN) study. We sought to evaluate long-term efficacy and safety of ozanimod.
MethodsWe examined data from an interim analysis of pts in the TN parent study who entered the ongoing TN open-label extension (OLE). Pts entered the TN OLE from the phase 3 TN study if they were non-responders at the end of induction, lost response during maintenance, or completed maintenance treatment, or from the phase 2 Touchstone OLE if they remained at study closure and received once-daily oral ozanimod 0.92 mg (equivalent to ozanimod HCl 1 mg). Clinical remission, clinical response, endoscopic improvement, and corticosteroid (CS)-free remission were evaluated at Wks 46, 94, and 142 in the TN OLE for all pts who entered the OLE from the TN parent study, and in the subset of pts in clinical response at the OLE entry. The data were analysed in the intent-to-treat population using observed cases (OC), which used the number of pts remaining in the study at the corresponding time point, and non-responder imputation (NRI), which used the number of pts remaining in the study at the corresponding time point and those who withdrew before the time point but would have reached the time point if they had stayed. Treatment-emergent adverse events were evaluated from the pooled phase 2 and phase 3 UC studies.
ResultsA total of 823 pts from TN entered the TN OLE; as of the cut-off date (Sept 30, 2020), 64% completed Wk 46, 34% completed Wk 94, and 14% completed Wk 142 of the OLE. The most common reason for discontinuation was lack of efficacy (21%). Baseline demographics were similar as in the TN study. A total of 261 pts were in clinical response at the time of OLE entry. OC analyses showed that the percentage of pts achieving clinical remission, clinical response, endoscopic improvement, and CS-free remission was maintained over time (Table). Efficacy in the responders was higher compared to the total population and was comparable within the endpoints at Wks 46 and 94. Using the more conservative NRI analysis, the proportion of pts achieving each endpoint was lower than in the OC; however, after 94 wks of OLE treatment, 34% of all pts and 55% of the responders still maintained clinical response. No new safety signals were seen with longer-term ozanimod use in the 1158 pts in the pooled population.
ConclusionUC pts from the phase 3 TN study demonstrated maintenance of response with long-term ozanimod treatment. These data reflect approximately 2 years of additional ozanimod treatment, with no new safety signals identified.
Protein tyrosine phosphtase non-receptor type 23 (PTPN23) plays a critical role in regulating epidermal growth factor (EGF) receptor signaling and its loss has been associated with aberrant cell proliferation and promotes onset of epithelial cancers. However, the role of PTPN23 in the intestinal epithelium has not been investigated yet. Here, we investigated how PTPN23 deletion in intestinal epithelial cells (IEC) affects intestinal homeostasis.
MethodsTo study the role of PTPN23 in the intestinal epithelium, we crossed mice with a LoxP flanked PTPN23 gene (PTPN23fl/fl mice) to mice expressing the CreERT construct under the villin promoter (PTPN23-VilCreERT mice). PTPN23 was deleted in IEC in these mice by tamoxifen-injections on five consecutive days. PTPN23 fl/fl mice injected with tamoxifen served as control.
ResultsPTPN23 deletion in IEC resulted in drastic loss of weight starting around 10-14days after the first tamoxifen injection, eventually leading to death within 3-5 weeks due to severe wasting disease with severe diarrhea. Histology revealed massive hyper-proliferation of the colonic epithelium accompanied with elevated immune cell infiltration. In line with previous reports on the function of PTPN23, we observed highly elevated levels of EGF receptor, possibly accounting for the massive epithelial hyper-proliferation and aberrant water secretion/defective water resorption in these mice. Furthermore, we observed bacterial translocation to the spleen and the liver, indicating defective anti-bacterial defense in the intestinal epithelium of PTPN23-VilCreERT mice. In line with this, 16S sequencing revealed significant differences in the intestinal microbiome with an overgrowth of bacteria that have been reported to be heavily coated with IgA. PTPN23-VilCreERT mice showed reduced apical presence of the poly Ig receptor, a receptor that transports IgA from the lamina propria through IEC into the gut lumen. Notably, while serum IgA levels were normal, its levels in the stool were reduced, confirming defective transport of IgA into the gut lumen. In addition, autophagy was significantly reduced in PTPN23-VilCreERT mice when compared to their littermates. Of interest, antibiotic treatment was sufficient to prevent epithelial hyper-proliferation, diarrhea and death in PTPN23VilCreERT mice, indicating that this drastic phenotype was microbiota-dependent and likely the result of defects in bacterial handling.
ConclusionOur results demonstrate that PTPN23 is indispensible for normal IEC function and its loss renders the intestinal epithelium unable to cope with invading bacteria. This uncovers a novel, so far unknown role of PTPN23 for regulating pathways involved in bacterial handling.
In a previous real-world study of long-term (up to 4 years) treatment with golimumab (GLM) in ulcerative colitis (UC), patients reported a low overall colectomy incidence (5.8%).1 This analysis evaluates the incidence of colectomy among patients with moderate-to-severe active UC in the PURSUIT-maintenance (-M)2 and long-term extension (-LTE)3 studies.
MethodsEligible PURSUIT-M trial participants completed a 6-week GLM induction trial without requiring colectomy.4,5 Responders to GLM induction were randomised 1:1:1 to GLM 50 mg, 100 mg, or placebo (PBO) maintenance for up to 1 year, administered every 4 weeks (q4w). Nonresponders to GLM or PBO induction received GLM 100 mg; responders to PBO induction received PBO (each administered q4w for up to 1 year). Participants experiencing loss of clinical response during maintenance were eligible for one treatment intensification (switch from PBO to GLM 100 mg, or GLM dose increase). Participants who completed PURSUIT-M were eligible to continue their treatment in the 3-year PURSUIT-LTE study. Colectomy (total or partial) was a prespecified outcome in PURSUIT-M; serious adverse event narratives and safety summaries were also examined for reports of colectomy (total or partial). For PURSUIT-LTE, serious adverse event narratives and safety summaries were examined for reports of colectomy (total or partial). The reasons for colectomy were not collected systematically in PURSUIT-M or -LTE. Descriptive information on colectomies was assessed and reported.
ResultsA total of 60 (4.9%) colectomies were reported among the 1228 patients who enrolled in the 1-year PURSUIT-M study, including 672 participants who continued into the 3-year LTE study. The table shows the distribution of colectomies by study phase, induction responder status, initial treatment assignment, and treatment prior to colectomy. The colectomy rate during the 3-year extension was lower than that observed during the maintenance phase of the study [1.3% (9/672) compared to 4.2% (51/1228)].
Consistent with previously reported data, this retrospective evaluation of colectomy data from the PURSUIT-M and -LTE studies in patients with moderate-to-severe active UC demonstrated a low occurrence of colectomy with long-term (up to 4 years) GLM treatment. The limited number of colectomies observed in the LTE study occurred predominantly in patients with more severe disease at baseline (induction non-responders) who had been receiving GLM 100 mg.
References:
1. Iborra M, et al. SciRep. 2020;10:17774
2. Sandborn WJ, et al. Gastroenterol. 2014;146:96–109
3. Reinisch W, et al. J Crohn's Col. 2018;12:1053–1066
4. Sandborn WJ, et al. Gastroenterol. 2014;146:85–95
5. Rutgeerts P, et al. Aliment Pharmacol Ther. 2015;42:504–514
In this real-world-evidence (RWE) study we aimed to analyse the persistence of biologic therapy in biologic-naïve ulcerative colitis (UC) patients and to compare 1-year effectiveness of vedolizumab (VDZ) and anti-TNF.
MethodsBetween 2017 and 2020, 1200 consecutively enrolled biologic-naïve and biologic- experienced patients with UC and Crohn´s disease (CD) were prospectively included in the VEDOIBD-Registry from 45 IBD-experienced centres across Germany. After exclusion of bio-experienced patients, CD and missing outcomes, the final sample consisted of 274 biologic-naïve UC-patients with 1-year follow-up data. Switchers of a drug were considered as treatment failure (modified intention-to-treat analysis; mITT) while switchers were excluded from per protocol analysis (PP). Clinical response modified (reduction of partial Mayo score (pMayo) from baseline to 1-year by >3 points or a reduction of at least 30% compared to baseline or reaching remission at 1-year) and (steroid-free) remission rates (pMayo ≤1 plus a bleeding subscore=0 (and no systemic use of steroids or budesonide at 1-year)) were predefined as outcomes. To reduce the effect of confounders, PS adjustment with inverse probability of treatment weighting (IPTW) was implemented. A weighted logistic regression was used, and the results were reported as odds ratio (OR) and 95% confidence interval (CI).
Results158 VDZ and 116 anti-TNF (ADA: 27.6%, IFX: 57.8%, GOL: 14.7%) biologic-naïve UC-patients were included in this prospective RWE comparing the effectiveness of VDZ vs anti-TNF. Until week 52 significantly more patients switched to another biologic-drug in the anti-TNF group than in the VDZ group (40.5% vs 16.5%; p<0.001) (Fig. 1). In mITT, clinical response at 1-year was significantly higher in VDZ than in anti-TNF treated patients (61.7% vs. 40.3%; OR 2.39 (95% CI 1.39-4.10)). VDZ also tended to be superior to anti-TNF for (steroid-free) remission (Tab. 1; p=0.058 (p=0.051)). In the PP-analysis, VDZ showed numerically higher 1-year effectiveness, but this did not reach statistical significance (Tab. 1). Analysing week-14 induction phase responders (Tab. 2), VDZ had numerically higher effectiveness rates compared to anti-TNF but without significant difference.
ConclusionThe 1-year maintenance findings suggested, in line with our previous induction phase data, only moderate long-term effectiveness in both groups. However, besides the significant response data, VDZ showed numerically higher remission rates compared to anti-TNF though only borderline significant. The higher treatment persistence of VDZ vs anti-TNF, along with the higher effectiveness, may suggest VDZ as a first-line biologic therapy option in UC patients.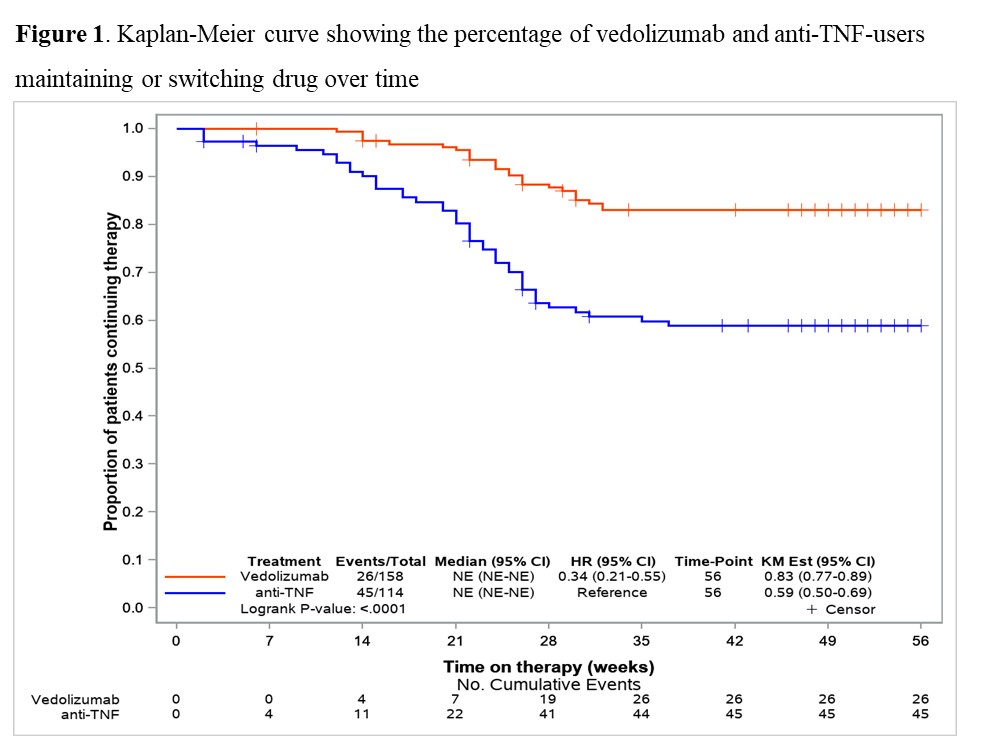


MDT case discussions
IBD Multidisciplinary Team (nurses, dietitians, pharmacists, psychologists, etc.)
1. To understand the chronicity of IBD and the need for continuous remission of symptoms
2. To review the drugs available to treat IBD, their indications, their limitations, their optimal use and their potential adverse reactions
3. To emphasise the concept of two goals of therapy which are the achievement of remission (induction therapy) and the prevention of disease flares (maintenance therapy)
4. To have an overview on the new drugs under development
Inflammatory Bowel Diseases are chronic diseases often with complex treatment. The treatment is lifelong and complex and may include several different pharmaceutical groups and sometimes surgery. Not rarely is treatment resistance developed and the treatment may come with different degrees of side effects. Earlier research has shown insufficient to medication adherence and a lower degree of health-related quality of life in patients with inflammatory bowel disease.
The aim is to describe the relationship between medication adherence and health-related quality of life in a Swedish population diagnosed with inflammatory bowel disease. Additional research questions are if any risk factors of low medication adherence can be identified from the collected variables.
MethodsThis cross-sectional study included N=206 patients from three different regions in Sweden. The questionnaires MMAS-8 and Short Health Scale were used combined with a questionnaire regarding patient characteristics. The data and patient characteristics were described and analyzed using descriptive statistics.
Ethical approval has been received from the Regional Ethical Review Board, Linköping, Sweden (no.: 2015/369-31).
The majority of patients had Ulcerative Colitis (62.6%) There were no significant differences between the different groups of Inflammatory Bowel Disease regarding patient characteristics apart from having gone through surgical procedures, which were more common in patients with Crohn’s disease. A small correlation was shown between medication adherence and the health-related quality of life dimension social function (rho = -0.146; p <0.05). Medication adherence showed no significant correlations to the remaining health-related quality of life dimensions: disease related worry, symptom burden and sense of general well-being. Possible risk factors identified for low medication adherence were age between 30 and 50, working at high occupational level, and higher educational level.
ConclusionThe complexity of measuring medication adherence has been established, making it difficult to make any certain conclusions regarding the hypothesis in this report. This study showed no clear association between medication adherence and health-related quality of life in patients with inflammatory bowel disease. However, it visualized the need of optimizing the instruments used to measure medication adherence in individuals with a non-conventional treatment plan
Numerous small molecules and biologics are being tested in phase 1-3 trials. Regarding JAK inihibitors, we still do not know whether JAK selectivity is associated with an improved risk-benefit profile, especially regading zoster risk. TYK2, gut selective or not, look promising and also showed very encouraging results in psoriasis. Other small molecules targeting integrins or PDE4 may be approbed in a near future. Regarding biologics and beyond biosimilars, many compounds are being developed such as Abivax. One question remains after 2 decades of biologics development : who will beat infliximab? Combination of biologics and bispecific antibodies might tackle this issue. Pending these molecules, many head to head trials are ongoing.
Chronic endoplasmic reticulum stress (ER) in the intestinal epithelium is a pathophysiological hallmark of IBD. cGAS/STING is an innate immune pathway involved in the detection of double stranded DNA fragments leading to the subsequent induction of type I IFN responses. We here tested the hypothesis that chronic ER stress impairs cGAS/STING signalling in the intestinal epithelium.
MethodsMice with a conditional intestinal epithelial deletion of Xbp1 (Xbp1ΔIEC, Xbp1fl/fl) were used to assess intestinal epithelial STING expression in-vivo. Small intestinal organoids (Xbp1ΔIEC, Xbp1fl/fl) and cell lines (Mode K, iCtrl and iXbp1) were used to assess cGAS/STING signalling in-vitro using STING agonist (dsDNA, DMXAA). Murine cytomegalovirus (mCMV) infection assays were performed in iCtrl and iXbp1cells and Xbp1ΔIEC, Xbp1fl/fl mice to functionally link impaired cGAS/STING to pathogen response. LC-MS profiling was performed in iCtrl and iXbp1cells to identify underlying metabolic programs affecting cGAS/STING responses in ER-stressed cells. IBD biopsy samples (cross-sectional, longitudinal therapy response cohort) were used to validate key molecular phenotypes in human IBD.
ResultsCompared to Xbp1fl/fl mice, Xbp1ΔIEC show completely abrogated STING expression in the basal crypt compartment of the small intestinal epithelium. In line with that iXbp1 ModeK cells displayed impaired pathway activation (TBK1) and interferon inducible gene expression (Cxcl10) in response to cGAS/STING stimulation and towards mCMV infection, leading to increased viral replication compared to iCtrl cells. In-vivo mCMV infection led to augmented small intestinal histopathological disease activity in Xbp1ΔIEC, but not Xbp1fl/fl mice. Using LC-MS, we show that ER-stress induces a metabolic adaptation towards increased serin/glycin metabolism, which is used to counterbalance reactive oxygen species (ROS) via glutathione (GSH) synthesis. Pharmacological interception of key pathways of GSH synthesis of deprivation of serin/glycin phenocopies ER-stress in abrogating STING signalling in IECs. Lastly, we show that key aspects of metabolic adaptation to ER-stress are present in intestinal biopsies of IBD patients.
ConclusionOur data describe a novel mechanism of metabolic adaptation to compensate ER-stress and maintain intestinal epithelial cGAS/STING signalling. We therefore put forward a model of ER-stress driven immunodeficiency via cGAS/STING signalling which renders the intestinal mucosa susceptible towards CMV infection in the context of IBD.
Educational objectives:
1. To understand the mechanism of action of Methotrexate
2. To review its efficacy and appropriate use (mono-, combitherapy)
3. To learn the appropriate management of Methotrexate and its potential adverse events in daily practice
4. To have an overview on other alternative indications
Educational objectives:
1) To demonstrate that IBD shares many endoscopic and histological features with other diseases.
2) To emphasize that the pathologist needs sufficient and qualitative clinical information to arrive at a correct diagnosis
Summary
Chronic inflammatory bowel diseases (IBD) are especially prevalent in Europe and North America. Their etiology and pathogenesis remain largely unknown.
IBD is diagnosed by a specialists' team consisting of gastro-enterologists, radiologists, surgeons, endoscopists, and pathologists.
The gastro-intestinal tract has however a limited number of responses to injury, therefore some conditions may simulate IBD clinically and histologically.
The mimickers of IBD fall in 4 groups:
1) Infections (particularly bacterial, but also viral, parasitic and fungal)
2) Specific and localized inflammations (e.g. diverticular colitis, endometriosis)
3) iatrogenic (including mainly drugs and medical interventions)
4) Other rare medical causes of IBD-like changes.
We have previously shown that treatment with mirikizumab (miri), a p19-directed IL-23 antibody, significantly downregulates inflammatory genes associated with disease activity and upregulates genes expressing epithelial transporter proteins in colonic tissue in patients with ulcerative colitis (UC). Here we explored the correlation between the expression of colonic mucosa genes and stool frequency (SF), a symptom reflective of disease activity, during the 12-week induction period of a Phase 2 study of patients with moderately to severely active UC (NCT02589665).
MethodsPatients were randomised 1:1:1:1 to receive intravenous placebo (PBO), miri 50mg or 200mg with possibility of exposure-based dose increases, or fixed miri 600mg every 4 weeks for 12 weeks. SF was reported daily by patients and transformed on a 4-level ordinal scale [0-3] representing increased SF above their normal or healthy baseline (BL). Patient colonic biopsies (PBO N=58, miri 50mg N=52, 200mg N=51, 600mg N=54) were collected at BL and Week (W)12, and gene expression measured using an Affymetrix HTA2.0 microarray workflow. BL and W12 gene expression or SF values were pooled and associations identified based on non-parametric Kendall’s tau. Pathway analysis (Hallmark and Reactome) of correlated genes was performed using over-representation analysis. p values of enrichment were determined by hypergeometric distribution test and adjusted for multi-testing with Benjamini-Hochberg procedure. Differential gene expression after miri treatment was determined by paired t-test comparing expression levels at BL and at W12 using data from the 200mg treatment group.
ResultsA total of 267 genes were correlated with SF (|tau| >0.3 and qval <0.001). Of these, 212 were positively correlated (high expression associated with high SF) and 55 were negatively correlated (high expression associated with low SF). The 212 transcripts that were positively correlated with SF were uniformly and consistently downregulated with miri treatment, while the 55 transcripts that negatively correlated with SF, were consistently upregulated with miri treatment (Table 1). Biological pathways significantly associated with the miri-responsive transcripts that correlated with SF included inflammatory response, extracellular matrix dysregulation, neutrophil degranulation and cytokine signaling pathways, especially TNF and IL6 pathways (Table 2).
ConclusionThis is the first study to identify colon-based transcripts that correlate with a clinical disease activity measure, stool frequency, and it demonstrates that treatment with miri may upregulate genes associated with normalization of SF and down regulate genes associated with inflammation in colonic tissue samples of patients with UC.

Long-term outcomes data after modified 2-stage ileal pouch anal anastomosis (IPAA), defined as completion proctectomy (CP) and IPAA without loop ileostomy, is lacking. We aimed to describe long-term functional results, patient satisfaction, and pouch survival in a cohort of patients from a high-volume center. We hypothesized selective m2-stage can result in comparable long-term pouch survival relative to a 3-stage approach.
MethodsOur institutional ileal pouch database was retrospectively reviewed to identify patients who underwent index IPAA surgery from 1983–2019. Adults >18 years of age who underwent CP with IPAA were included. At our specialized institution, m2-stage is performed selectively based on surgeon judgement. Patients were stratified into 2 groups (3-stage vs m2-stage) and matched on a 1:1 basis based on age ±5, year of operation ±3, gender, preoperative diagnosis, double-stapled vs handsewn, and laparoscopy. Primary outcome was pouch survival, with pouch failure defined as permanent diversion, pouch excision, or conversion to a Kock pouch.
ResultsIn total, 2,433 patients were included, of whom 2,198 (90.3%) underwent 3-stage IPAA and 235 (9.7%) m2-stage IPAA. Matching resulted in 223 matched pairs, and long-term pouch survival (95.5% vs 93.2%, p=0.32) did not significantly differ (Figure 1). Short-term outcomes in the matched pairs revealed a shorter postoperative length of stay in the 3-stage patients (5 vs 8 days, p<0.001), but no significant difference in postoperative complications (12.1% vs 17%, p=0.09) was seen between the matched 3-stage and m2-stage patients, respectively. Functionally, there was no difference in the number of stools/24 hours (7 vs 7, p=0.33) or in proportion of patients requiring seepage protection at night (29.7% vs 24.6%, p=0.31). However, 3-stage patients required significantly more seepage protection during the day (25.1% vs 15.0%, p=0.02). Regarding pouchitis, there was no difference in the proportion of patients reporting recent symptoms (33.4% vs 33.3%, p=1.0), episodes in the last year (0 vs 0, p=0.51), or pouchitis requiring continuous medication (16.7% vs 10.1%, p=0.10). Patient satisfaction was similar as no difference in the proportion of those who would have surgery again (90.4% vs 93.7%, p=0.34), those who would recommend surgery (94% vs 95.5%, p=0.68), or overall patient satisfaction with surgery on a scale of 1 – 10 (highest) (3 vs 7, p=0.07) was reported.
Figure 1: Kaplan-Meier curve for pouch survival (matched pairs)
Long-term outcomes were similar in patients who underwent modified 2-stage and 3-stage IPAA. Modified 2-stage IPAA is an alternative for selected patients with limited options if performed at high-volume centers in experienced hands.
Summary of the talk
Timely limitation of the inflammatory process is essential, because its self-perpetuation will otherwise lead to the onset of complications and disease progression. In contrast to inflammatory processes, resolution of inflammation and molecular healing are far less well understood in IBD. In-depth characterization of pathways that terminate inflammation and lead to molecular healing has been incomplete to date. Resolution of inflammation involves several active processes rather than just a stepwise clearance of pro-inflammatory mediators. Recent studies have shown that blockade of just one of the pro-inflammatory mediators might be circumvented by the activation of alternative, redundant pro-inflammatory pathways, thus leading to loss of response. An improved understanding of these resistance mechanisms would help us to improve our currently used therapeutic strategies and reveal new treatment targets and concepts. Our future therapeutic aim should be the restoration of mucosal homeostasis and resolution of all perturbed molecular components (e.g. activation of immune cells, perturbed epithelial barrier integrity and disturbed antigen tolerance). This kind of molecular healing might minimize the risk for relapses and lead to lasting control of the disease.
1.) To understand mechanisms that are involved in the resolution of inflammation and molecular healing in IBD
2.) To get an overview on identified molecular resistance mechanisms to biological therapies and how they could be therapeutically utilized
3.) To understand how molecular healing could be defined in IBD
