Interactive cases will be presented to illustrate IUS diagnosis of UC complications, such as acute severe colitis, including monitoring of response to treatment, perforation, chronic structural damage in UC, infectious colitis, pseudopolips and lymphoma.
Crohn’s disease (CD) is predominantly allocated within the small bowel and characterized by persistent chronic inflammation that may cause an extramural complications. Intestinal Ultrasound (IUS) has shown to be highly effective in detecting and determining CD related complications such as Strictures, fistulas, and inflammatory masses. The aim of this interactive presentation is to show the use of IUS in some real clinical cases.
Inflammatory bowel disease (IBD) is a complex disease characterised by chronic inflammation of the digestive tract. Genome-wide association studies (GWAS) have identified 241 risk loci significantly associated with the two common forms of IBD, Crohn’s disease and ulcerative colitis. The vast majority of these risk loci reside in non-coding regions of the genome, and we only know which gene is dysregulated to increase risk of disease for a minority. This knowledge gap makes it difficult to draw insights into disease pathology and identify new candidate drug targets.
MethodsTo improve biological insights from IBD GWAS, we generated single cell RNA-sequencing data from ileal biopsies ascertained from 25 CD patients with active ileal inflammation and 26 non-IBD controls. We identified 49 different cell types among the ~140K sequenced cells (Fig.1), including all major immune, enterocyte, secretory and mesenchymal populations. Our optimized single-cell dissociation protocol preserves the top of villus epithelial cells, which are inherently prone to anoikis, enabling generation of high-quality transcriptomes for the first time. 
Fig. 1
Single-cell atlas of terminal ileum biopsies from Crohn’s disease and non-IBD individuals.
We identified 797 unique genes differentially expressed between CD patients and controls, with notable expression differences in stem cell, secretory, and enterocyte populations. Genes involved in antigen presentation and interferon-gamma signaling were enriched among those most frequently dysregulated cell types. In an attempt to identify which of these expression differences are likely causal of disease, rather than simply a consequence of it, we integrated results from the latest IBD GWAS to assess the extent to which genes captured disease heritability, and in which cell-types. Genes specifically expressed in Tregs, monocytes and IL10RA-negative monocyte-derived macrophages captured a significant fraction of disease heritability, strongly implicating these cell types in disease pathogenesis. We investigated which genes were driving these enrichment signals and identified candidate effector genes at many IBD risk loci. Reassuringly, many confirmed IBD effector genes known to have a role in the normal functioning of these cell types were found, including NOD2, IL18RAP, IL23R, NCF4, and IL2RA.
ConclusionSingle-cell analysis combined with IBD genetics has generated strong evidence for a causal role of novel disease mechanisms that have therapeutic potential. Further experiments are underway to validate this finding. At ECCO we will present an updated version of this analysis, including genetic mapping of gene-regulation across cell types to identify IBD effector genes and causal variants.
Environmental factors play an important role in the pathogenesis of IBD. Thereby the question: can we modulate these factors and impact the disease course?
A lifestyle change including physical activity and diet can be beneficial for patients with IBD.
The main objective of this presentation is to review recent data from intervention trials supporting this lifestyle change in patients with IBD.
T resident memory (Trm) cells in the intestinal mucosa and in particular subpopulations expressing phenotypic markers such as alphaE-beta7 or NKG2D have been associated with chronic inflammatory bowel disease (IBD) activity. We hypothesize that these populations may have a direct deleterious impact on the intestinal epithelium in IBD.
MethodsThe phenotypic study of mucosal lymphocytes was performed in two prospective cohorts: ELYP including patients with active IBD before initiation of biotherapy and REMIND including patients with ileal Crohn's disease (CD) requiring ileocaecal resection. These analyses were performed before initiation of treatment and one year after continuous therapy in the ELYP cohort and on the resection specimen in the REMIND cohort. An innovative ex vivo autologous organoid-mucosal T cell coculture model was developed using the REMIND cohort specimens for patients and healthy ileum from individuals without IBD for controls (Figure 1). T cell infiltration within the organoid and epithelial cell death were assessed by confocal microscopy. A panel of 30 cytokines was quantified in the supernatants of cocultures.
Figure 1
In the ELYP cohort, before the start of treatment, IBD patients had lower expression of alphaE-beta7 and NKG2D on mucosal CD8 T cells. While alphaE-beta7 and NKG2D expression on mucosal CD8 T cells had returned to normal in endoscopic responders, it remained decreased in non-responders. Similarly, the inflammatory mucosa of the REMIND surgical specimens had lower levels of CD4 and CD8 T cells expressing alphaE-beta7 and NKG2D compared with controls and non-inflamed regions. We developed a coculture model between mucosal lymphocytes and organoids generated under autologous conditions. We showed an increase in apoptotic cell death in epithelial cells from CD patients which was not found in control cocultures. There was a significant correlation between the degree of epithelial cell death and T cell infiltration (Figure 2). Various proinflammatory cytokines such as IFNgamma, TNFalpha, IL-6 and IL- 17a were also increased in the supernatants. The use of antibodies blocking the alphaE-beta7 and NKG2D pathways of interest inhibited this effect by different mechanisms (Figure 3) While anti-beta7 and anti-NKG2D had comparable effects in terms of cell death inhibition, only anti-beta7 reduced T cell infiltration. Anti-NKG2D had no effect on cell infiltration but a reduction of perforin was observed in the supernatants.
Figure 2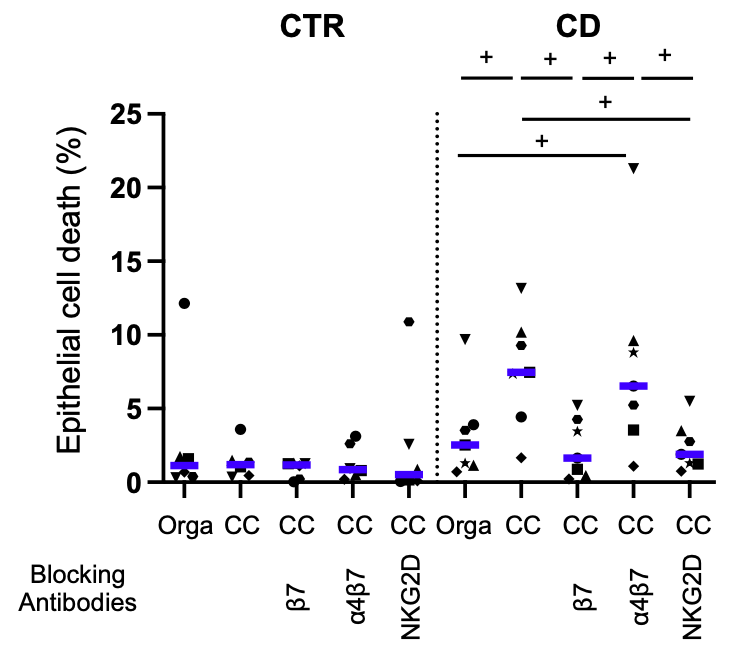
Figure 3
CC= Coculture
These data demonstrate for the first time the direct cytotoxic deleterious effect of mucosal T cells on the epithelium of CD patients using a novel coculture model. AlphaE-beta7 and NKG2D pathways appear to be relevant in this process.
The disease course of inflammatory bowel disease (IBD) is heterogeneous and highly unpredictable. Intestinal Ultrasound (IUS) is a non-invasive modality capable of assessing disease activity in IBD. IUS is reliable, patient-friendly, and allows frequent monitoring of disease activity. However, the evidence for IUS as a predictor of disease course is still limited. Here we present novel data on the predictive value of IUS performed at the time of IBD diagnosis.
MethodsPatients with new-onset IBD are currently being included in the ongoing multicentre prospective inception cohort study, the IBD Prognosis Study. During the first five years following diagnosis, patients undergo regular clinical, biochemical, endoscopic, and imaging assessments. IBD treatment and disease events are prospectively recorded. IUS is performed at diagnosis, after three months, and hereafter annually. Patients with proctitis do not undergo assessment with IUS. The newly developed IUS score, the International Bowel Ultrasound Segmental Activity Score (IBUS-SAS), is calculated for the most inflamed segment, with a high score indicating severe disease activity. The score incorporates bowel wall thickness (BWT), bowel wall stratification, colour Doppler signal, and inflammatory fat. In this abstract, we report our preliminary results after including patients for six months.
ResultsIBUS-SAS at diagnosis was available in 60 patients. 32 patients were diagnosed with Crohn’s disease (ilieal: 7, colonic: 19, ileocolonic: 6) and 28 patients were diagnosed with ulcerative colitis (UC) or unclassified IBD (proctitis: 1, left-sided colitis: 8, extensive colitis: 19). The mean IBUS-SAS at diagnosis was 51.1, with a mean BWT of 5.2 mm. Major clinical outcomes were initiation of biologic therapy, n=12 (20.0%), IBD-related bowel resection, n=5 (8.3%), IBD-related hospitalisation, n=19 (31.7%). The mean IBUS-SAS at diagnosis was 66.2 among patients with the combined endpoint of any of these disease outcomes during follow-up vs. 34.7 for no major outcomes (p<0.001), see Figure 1. Additionally, we found that all patients with an IBUS-SAS above 80 at diagnosis had been hospitalised and started on systemic steroids. So far, 20 patients had an IUS follow-up scan after three months showing a mean IBUS-SAS reduction by 17.0 points (p=0.008).
We present data on the predictive value of early IUS in new-onset IBD. IUS activity at diagnosis of IBD seems to have the capability to predict short term disease outcome. At diagnosis, high IBUS-SAS is associated with major disease events such as starting biological therapy, IBD-related bowel resection, and IBD-related hospitalisation. Furthermore, response to treatment is reflected by a decrease in IBUS-SAS after three months.
Educational objectives:
- Identify casual roles for diet in developing IBD.
- Present research on how having IBD might impact diet.
- Discuss ways to separate these effects in order to improve diet management for IBD patients.
Summary:
The link between diet and IBD is well-established. Most of the focus, especially over the last few years, has been on how diet might lead to or trigger the development of IBD, and use of diet as a therapy, especially in shown for paediatric Crohn disease. Both epidemiologic research and animal/mechanistic studies support beneficial (e.g., fruits and vegetables) and detrimental (e.g., processed foods) roles of foods in developing IBD. However, having IBD certainly impacts one’s diet; this could include avoidance of food overall, foods that increase symptoms, or following advice from clinicians. This bidirectional relationship complicates our ability to understand the relationship between diet and IBD and guide patient care.
In this presentation I will discuss this topic and offer ways to better define the link between diet and IBD. There are certainly misconceptions and confusing messages related to diet management for IBD patients as a result of this 2-way relationship. It is important for both dietitians and those involved in diet research in IBD to be aware of these factors and find ways to improve diet research and patient care.
Learning Objectives:
1. Drug safety at conception and during pregnancy
2. Management of disease exacerbation during pregnancy, assessment and therapeutic options
3. Management of biologics during pregnancy and post-partum
Educational objectives:
1. Learn about the mechanisms of action of tofacitinib
2. Understand the clinical and endoscopic efficacy of tofacitinib in UC
3. Discuss the safety profile of tofacitinib
Immune responses to the SARS-CoV-2 vaccination may be influenced by immunomodulatory drugs (IMDs). We investigated the immune responses and safety in fully vaccinated Japanese patients with IBD.
MethodsIBD patients and control subjects at 39 institutes were invited to participate in the study from March to October 2021. Blood sample collections to measure anti-SARS-CoV-2 spike IgG antibody titers were planned pre-1st vaccination, pre-2nd vaccination, and at 4 weeks, 3 months and 6 months post-2nd vaccination. Immune responses were compared between groups, considering baseline characteristics and IMD treatments. (UMIN000043545) The interim analyses presented here include mainly data from the 4-weeks post-2nd vaccination time-point.
ResultsIn total, 679 IBD patients and 203 controls were enrolled (Table 1). The IBD group received the BNT162b2 vaccine (86.2%) and the mRNA-1273 vaccine (12.5%), and the control group received the BNT162b2 vaccine (86.9%) and the mRNA-1273 vaccine (12.1%). Only 4 cases (0.7%) in the IBD group and 2 (1.0%) in the control group were infected with COVID-19. Adverse events of 2nd vaccination occurred in 48.4% of the IBD group and 35.1% of the control group. Comparison between administrated and non-administrated IBD patients for each IMD revealed an attenuated genomic mean titer (GMT [U/mL]) in those taking systemic steroids (18.85 vs 31.24), anti-TNF monotherapy (28.31 vs 42.99), anti-TNF therapy+ immunomodulator (IM) (12.86 vs 35.26), vedolizumab+IM (19.49 vs 30.39), ustekinumab+IM (20.44 vs 30.79), and tofacitinib (9.54 vs 32.08), but not in those taking oral 5-ASA (29.50 vs 32.40), or vedolizumab (41.85 vs 40.20) and ustekinumab (55.56 vs 39.26) monotherapies. Estimated least square means of the GMT by a multiple linear regression model are shown in Table 2. GMTs were significantly influenced by increasing age and allergy (51.2, 95%CI 42.1-62.3; p=0.0293), and tended to be influenced by COVID-19 infection (139.1, 41.0-472.2; p=0.0572). Sex, smoking, drinking, IBD, and adverse events of 2nd vaccination did not affect the GMT. The GMT was significantly higher for mRNA-1273 (90.3 [60.8-134.1]) than for BNT162b2 (39.6 [35.2-44.6], p= 0.0001). Systemic steroids (22.9 [13.9-37.7], p=0.0119), IM (24.2 [18.7-31.4], p<0.0001), anti-TNF agents (20.8 [15.3-28.3], p<0.0001), vedolizumab (25.2 [15.0-42.2], p=0.0409), ustekinumab (28.9 [18.5-45.0], p=0.0754), and tofacitinib (5.5 [2.8-10.9], p<0.0001), but not oral 5-ASA (39.1 [31.9-47.9], p=0.3225), attenuated GMTs at 4 weeks post-2nd vaccination (Table 2).

Aging and most IMD options attenuated immunogenicity in fully vaccinated IBD patients. Prioritization of a booster vaccination should be considered for IBD patients treated with IMDs.
The Kono-S anastomosis is a novel method of anastomosing the bowel after a Crohn's resection. It may reduce the incidence of recurrent disease. The talk will cover
-The purpose of the technique
-How to do it
-How it may work
- Evidence for safety and efficacy
-How it may be improved
This talk aims to answer five key questions relating to covid-19 and Inflammatory bowel disease.
(1) Are patients with inflammatory bowel disease (IBD) at increased risk of COVID-19?
(2) Are IBD patients with COVID-19 at increased risk of adverse events?
(3) What is the impact of IBD medications on risk of COVID-19?
(4) Does COVID-19 impact IBD disease activity?
(5) What are latest data and guidance on COVID-19 vaccines in IBD?
COVID-19 is the disease caused by the SARS-CoV-2 virus, but overall patients with IBD do not appear to be at a higher risk for infection with SARS-CoV-2 or development of COVID-19. Current data suggest that certain IBD patients with COVID-19 may be at increased risk of adverse events and this risk is primarily driven by older age, comorbidities, disease activity and steroid use. Data from a community study in the USA and the SECURE registry showed that prednisone use increases risk of severe COVID-19 whereas use of biologics/small molecule inhibitors, immunomodulators, or combination therapy does not. Hence patients with IBD who do not have infection with SARS-CoV-2 should not discontinue their IBD therapies. COVID-19 does not appear to have durable impact on IBD disease activity. Patients with IBD who develop COVID-19 should be managed on a case-by-case basis. The severity of the COVID-19 and the severity of the IBD should result in careful risk–benefit assessments regarding treatments for COVID-19 and escalating treatments for IBD.
International guidelines encourage IBD patients to get the COVID-19 vaccine. Currently there are no apparent risk of IBD flare with COVID-19 vaccine and side effects are similar to the general population. In IBD patients the immunogenicity of COVID-19 vaccines is differentially impacted by immunosuppressive drugs. The CLARITY study showed that Infliximab is associated with attenuated antibody responses following 3 vaccine doses. Breakthrough SARS-CoV-2 infections (and re-infections) are more common and occur earlier in infliximab-treated patients, irrespective of initial vaccine type. A recent study from the UK showed that COVID-19 vaccine-induced antibody responses are impaired in IBD patients treated with infliximab or tofacitinib, but not thiopurines, ustekinumab or vedolizumab. Scheduling of third primary, or booster dosing could be personalised based on individual’s treatment and patients taking anti-TNF or Tofacitinib should be prioritised.
2) Limited data in nich IBD indications and how to deal with it?
3) The introduction of subcutaneous formulation while many practical questions remain
4) Safety aspects of well known and more novel advanced therapies
5) Economical aspects
In this talk will be shown that the efficacy of medical therapy in order to close perianal fistula is low, and if successful, that only the external opening is closed (clinical closure)
Only medical therapy in combination with surgical closure can truly heal the fistula as shown by MR (radiological closure). Radiological closure is associated by a superior PDAI and must be the goal of treatment. Clinical closure is characterized by inferior PDAI, reopening of the fistula tract and more reinterventions.
So, preferably, fistula amenable for surgical closure, should be attempted to close surgically after optimizing medical therapy.
Primary sclerosing cholangitis is a chronic cholestatic disorder with a high impact on quality of life and patient survival in children with concomitant IBD. Adult and pediatric PSC present with different characteristics, specifically an increased risk of PSC in adults (a fivefold higher incidence of the disease in adults than children); the more common occurrence of small duct disease in children compared to adults; and a more frequent overlap of autoimmune hepatitis in children as compared to adults. It is still unclear if pediatric PSC should be considered a different disease than adult-onset PSC or an early presentation of the same disease. The etiology of PSC is still unknown, but several mechanisms have been hypothesized, including genetic predisposition, altered immunologic response, and gut microbiome or metabolome modifications on the biliary epithelium. A better understanding of the pathogenic mechanisms would eventually help future therapies and allow precise identification of the cause and course of the disease in both adults and children. IBD-PSC lacks specific therapies, although immunomodulator therapy can be used for the autoimmune hepatitis component of pediatric PSC. Published data suggest that children with IBD-PSC are not at a higher risk for hepatobiliary cancers. However, surveillance programs applied in adults are generally indicated in children too. The risk of colon cancer seems similar to that reported in adults; therefore surveillance is mandatory. Median transplant-free survival and patient survival after liver transplant for PSC seem similar in the pediatric and adult-onset PSC. So far, there is no effective long-term therapy for PSC, and liver transplantation remains the only life-extending treatment.
Sphingosine-1-phosphate (S1P) receptor modulators may be associated with bradycardia and atrioventricular conduction delays. A previous analysis demonstrated first-dose ozanimod had minimal effects on cardiac function, including in patients (pts) with a known history of cardiovascular disease. This analysis evaluated long-term cardiac safety following continuous ozanimod treatment from the phase 3 ulcerative colitis (UC) True North trial and multiple sclerosis (MS) 12-mo SUNBEAM and 24-mo RADIANCE trials.
MethodsOzanimod 0.92 mg (equivalent to ozanimod HCl 1 mg)–treated pts from True North and pooled SUNBEAM/RADIANCE trials were included. In True North, pts in Cohort 1 received double-blind ozanimod or placebo and pts in Cohort 2 received open-label ozanimod in the induction period; in the maintenance period, pts with clinical response to ozanimod at 10 weeks were rerandomized to double-blind ozanimod or placebo. In True North, ECGs were monitored at screening, day 1, wk-10, and wk-52; heart rate (HR) was monitored at every visit. In the MS trials, ECGs were monitored at screening, baseline, day 15, and end of treatment (EOT); HR was monitored similarly at the beginning, then every 3 mo until EOT. Cardiac-related treatment-emergent AEs (TEAEs) were reported.
ResultsIn the UC trial, continuous ozanimod treatment was not associated with any clinically significant changes in HR or ECG. The incidence of cardiac-related TEAEs with ozanimod during induction in Cohorts 1 and 2 was low (Table). In maintenance, cardiac-related TEAEs were reported in 1.3% (3/230) of pts in the continuous ozanimod group (Table); incidence was numerically higher in ozanimod pts with (2 of 57 pts [3.5%]) versus without (1 of 173 pts [0.6%]) prior history of cardiovascular disease. Cardiac-related serious AEs (SAEs) were uncommon (angina pectoris, coronary artery stenosis, pericarditis in 1 patient each). In the pooled MS studies, no clinically significant HR or ECG changes were associated with chronic treatment up to mo 24. The incidence of cardiac-related TEAEs was low with ozanimod (Table); incidence was similar among pts with (6 of 171 pts [3.5%]) versus without (24 of 711 pts [3.4%]) prior history of cardiovascular disease. Two of 882 patients experienced cardiac-related SAEs resulting in hospitalization with ozanimod in the MS studies (asymptomatic sinus bradycardia [HR 44 bpm] and symptomatic supraventricular tachycardia).
ConclusionOzanimod had a manageable long-term cardiac safety profile with a low incidence of bradycardia and few serious long-term cardiac safety findings in the phase 3 UC and MS ozanimod trials.

The vast majority of patients with ulcerative colitis (UC) and Crohn’s disease (CD) who acquire coronavirus disease 2019 (COVID-19) survive the infection. Still, the long-term health consequences of COVID-19 are not well described in patients with underlying inflammatory bowel disease (IBD).
MethodsWe conducted a population-based study investigating the outcomes of COVID-19 among patients with UC and CD in Denmark. The Danish COVID-19 IBD Database is an extensive population-based database which prospectively monitors the disease course of laboratory-confirmed COVID-19 among patients with UC and CD. Severe COVID-19 was defined as COVID-19 necessitating intensive care unit admission, ventilator use, or death, while adverse COVID-19 was defined as requirement of COVID-19 related hospitalization. Sequelae following COVID-19 were defined as symptoms that developed during or after an infection consistent with COVID-19, were present for more than 12 weeks, and were not attributable to alternative diagnoses.
ResultsThe study included 319 patients with UC and 197 patients with CD from January 28th, 2020, to April 1st, 2021. Of these, a total of 137 (42.9%) and 85 (43.1%), respectively, participated in a subsequent investigation of post-COVID-19 sequelae after a median of 5.1 months (IQR 4.5-7.9) after infection (Table 1). An equal proportion of patients with UC (58 (42.3%)) and CD (39 (45.9%), p=0.60) reported persisting symptoms of COVID-19 for at least 12 weeks, consistent with the development of post-COVID-19 syndrome. The most common persisting patient-reported symptoms included fatigue (UC: 49 (35.8%), CD: 31 (36.5%), p=0.92), anosmia (UC: 37 (27.0%), CD: 25 (29.4%), p=0.70), ageusia (UC: 26 (19.0%), CD: 24 (28.2%), p=0.11), headache (UC: 19 (13.9%), CD: 16 (18.8%), p=0.32), dyspnea (UC: 19 (13.9%), CD: 16 (18.8%), p=0.32), and arthralgia (UC: 17 (12.4%), CD: 14 (16.5%), p=0.40) (Figure 1). Only discontinuation of immunosuppressive therapies for UC during COVID-19 (OR=1.50 (95% CI 1.07-10.22), p=0.01) and the severity of COVID-19 among patients with CD were independently associated with the long-term effects of COVID-19 (OR=2.76 (95% CI 1.05-3.90), p=0.04) (Tables 2-3).



 Conclusion
ConclusionThis Danish population-based study found a high occurrence of patient-reported persisting symptoms following the acute phase of COVID-19 infection, which were associated with the discontinuation of immunosuppressive therapies for UC during COVID-19 and the severity of COVID-19 among patients with CD. These findings might have implications for planning the healthcare of patients with inflammatory bowel diseases in the post-COVID-19 era.
